20 Ulnar Neuropathy at the Wrist
Ulnar neuropathy at the wrist (UNW) is a rare condition that sometimes is confused with ulnar neuropathy at the elbow (UNE) or, more often, with early motor neuron disease. Knowledge of the detailed anatomy of the ulnar nerve at the wrist is necessary to understand the several unique clinical and electrophysiologic patterns that can occur with UNW (Figure 20–1).
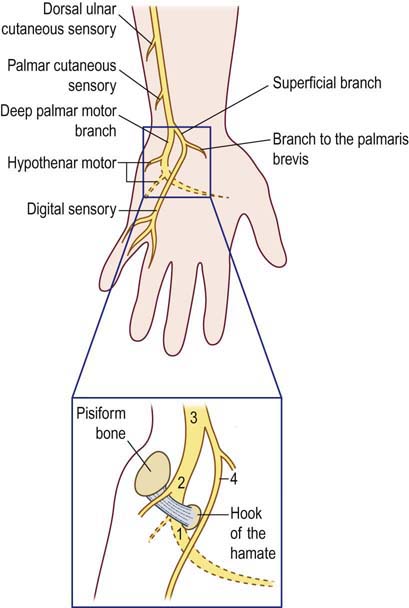
FIGURE 20–1 Detailed anatomy of the ulnar nerve at the wrist.
Entrapment of the ulnar nerve at the wrist can take on several patterns: (1) pure motor affecting only the distal deep palmar motor branch, distal to the hypothenar muscles, (2) pure motor affecting the proximal deep palmar branch including the hypothenar motor branches, (3) motor and sensory (proximal canal lesion), and rarely (4) sensory affecting the superificial branch involving the sensory fibers to the volar fourth and fifth fingers. The superficial branch does supply one muscle, the palmaris brevis. This muscle, however, is difficult to assess clinically or by EMG, although there are reports of the “palmaris brevis sign” wherein this muscle is spared or prominent in lesions of the deep palmar motor branch (see Figure 20–2).
(Adapted with permission from Olney, R.K., Hanson, M., 1988. AAEE case report no. 15: ulnar neuropathy at or distal to the wrist. Muscle Nerve 11, 828.)
Clinical
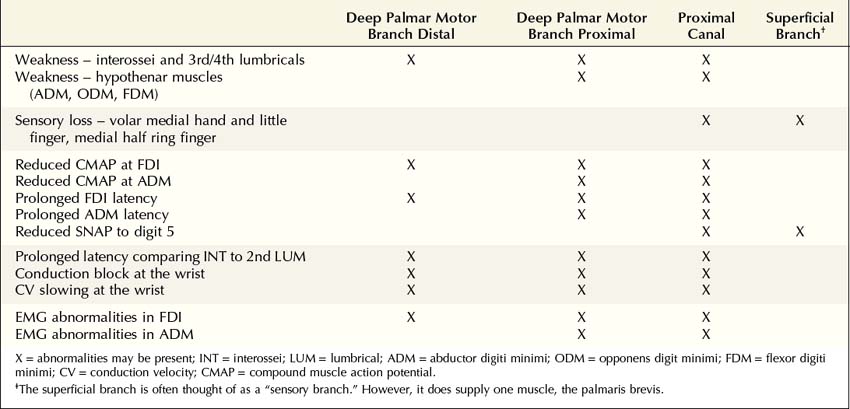
Several subtypes of UNW occur, depending on the exact location of the lesion and which fibers are affected (Table 20–1 and Box 20–1). The following lesions have been described:
• Distal deep palmar motor lesion: Affects all muscles supplied by the deep palmar motor branch except the hypothenar muscles; the superficial branch containing the sensory fibers and motor innervation to the palmaris brevis is not affected.
• Proximal deep palmar motor lesion: Affects all ulnar-innervated hand muscles, including the hypothenar muscles, with the exception of the palmaris brevis; the superficial branch containing the sensory fibers and motor innervation to the palmaris brevis is not affected.
• Proximal canal lesion: Affects all branches of the ulnar nerve, including the proximal and distal deep palmar motor and the superficial branches which contain the sensory fibers and motor innervation to the palmaris brevis.
• Superficial branch lesion: Affects only the superficial branch, which is primarily sensory. Note that while the palmaris brevis muscle is affected, this is not clinically apparent.
Table 20–1 Clinical and Electrophysiologic Differentiating Factors in Variants of Ulnar Neuropathy at the Wrist
Box 20–1
Clinical and Electrophysiologic Abnormalities not Consistent with Ulnar Neuropathy at the Wrist
Clinical
• Weakness of thumb abduction (abductor pollicis brevis – median innervated)
• Weakness of the finger flexors of digits 4 and 5 (flexor digitorum profundus – ulnar innervated in the forearm)
• Weakness of index finger extension (extensor indicis proprius – radial innervated)
• Sensory symptoms/signs in the dorsal medial hand/dorsal fifth and fourth fingers (territory of the dorsal ulnar cutaneous sensory branch)
• Sensory symptoms/signs in the medial forearm (territory of the medial antebrachial cutaneous sensory nerve)
The first two patterns are the most common, accounting for more than 75% of all cases of UNW. In both, the superficial branch is not affected; thus, there are no sensory symptoms or sensory loss. Patients present with painless weakness and atrophy of ulnar intrinsic hand muscles. Because the ulnar-innervated adductor pollicis and deep head of the flexor pollicis brevis are in the thenar eminence, both the hypothenar and thenar eminences may be wasted, if the lesion is in the proximal deep palmar motor branch. Similar to UNE, the Benediction hand posture, Froment’s sign, and Wartenberg’s sign may be present in advanced cases. In addition, another somewhat obscure sign, known as the “palmaris brevis sign,” may be seen in severe lesions of the deep palmar motor branch. Remember that the palmar brevis is the only muscle supplied by the superficial branch, and is therefore spared in lesions of the deep branch. When the palmaris brevis contracts, it results in puckering of the skin along the proximal medial border of the hand. Because the other intrinsic hand muscles are wasted, prominent contraction (and possibly hypertrophy) of the palmaris brevis may be seen when the fifth digit is forcibly contracted in the more common lesions of the deep palmar motor branch of the ulnar nerve at the wrist (the “palmaris brevis sign,” Figure 20–2).
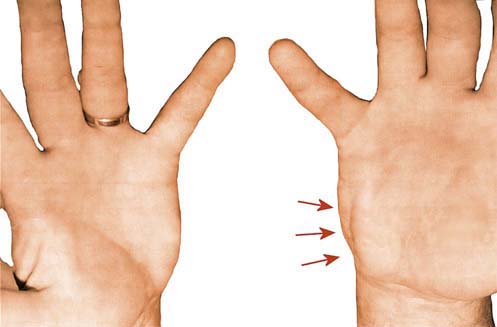
FIGURE 20–2 Palmaris brevis sign.
(Adapted with permission from Iyer, V.G., 1998. Palmaris brevis sign in ulnar neuropathy. Muscle Nerve 21, 675–677.)
Etiology
Entrapment of the ulnar nerve at the wrist is far less common than at the more usual sites at the elbow. It has been described in association with trauma and wrist fracture. However, more common is a ganglion cyst within Guyon’s canal that compresses the ulnar nerve (Figure 20–3). Rarely, an anomalous muscle or other mass lesions have been reported, including ulnar artery aneurysms, lipomas and other tumors. In addition, certain occupations or activities that involve repetitive movement or pressure against the ulnar wrist predispose to lesions at this location. This is especially true for bikers or laborers who use the same hand tools repetitively, which results in pressure on the hypothenar eminence (Figure 20–4). In such patients, the hypothenar area may be calloused at the compression site.
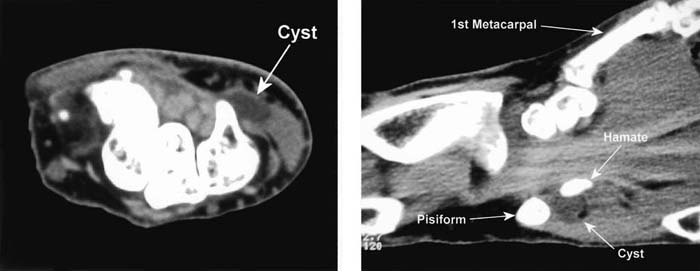
FIGURE 20–3 Ganglion cyst in Guyon’s canal.
(From Preston, D.C., Shapiro, B.E., Schecht, H.M., 2001. Ganglion cyst at Guyon’s canal: electrophysiology and pathology. J Clin Neuromusc Dis 3, 89–91.)
Differential Diagnosis
In lesions where the superficial branch containing the sensory fibers is not affected, UNW is most often confused with early motor neuron disease. Motor neuron disease is well known to present with painless atrophy and weakness of a distal limb, a pattern essentially identical to distal UNW lesions. The key differentiating finding on physical examination in UNW is the intact strength and bulk of the abductor pollicis brevis muscle, supplied by the median nerve. In motor neuron disease, one would expect all C8–T1-innervated muscles to be equally affected. In UNW, there is a marked difference between ulnar C8–T1-innervated muscles (which are weak and wasted) and median C8–T1-innervated muscles (which are spared). However, this difference in ulnar versus median innervated muscles can also be seen in some atypical motor neuron disorders, such as multifocal motor neuropathy with conduction block, a rare autoimmune mediated motor neuropathy that preferentially affects distal muscles in a non-myotomal pattern of weakness (see Chapter 26).
Electrophysiologic Evaluation
Nerve Conduction Studies
The findings on nerve conduction studies in UNW depend on (1) whether the superficial sensory branch is involved and (2) if the deep motor branch is involved, whether it is affected proximal or distal to the hypothenar muscles. If the lesion is distal, affecting only the deep palmar motor branch after the take-off to the hypothenar muscles, then the routine ulnar sensory study, recording the fifth digit, and the routine ulnar motor conduction study, recording the ADM, will be normal. In suspected UNW, additional nerve conduction studies must always be performed in order to detect abnormalities that may not be present on routine ulnar motor and sensory studies (Box 20–2).
Box 20–2
Recommended Nerve Conduction Study Protocol for Ulnar Neuropathy at the Wrist
1. Ulnar motor study recording abductor digiti minimi, stimulating wrist, below groove, and above groove in the flexed elbow position
2. Ulnar motor study recording first dorsal interosseous, stimulating wrist, below groove, and above groove in the flexed elbow position
3. Ulnar motor study recording first dorsal interosseous, stimulating the wrist (3 cm proximal to the distal wrist crease) and palm (4 cm distal to the distal wrist crease)
4. Median motor study recording abductor pollicis brevis, stimulating wrist and antecubital fossa
5. Median and ulnar F responses
6. Ulnar sensory response, recording digit 5, stimulating wrist (bilateral studies)
7. Median sensory response, recording digit 2 or 3, stimulating wrist
8. Dorsal ulnar cutaneous sensory response (bilateral studies)
Additional studies to consider:
9. Ulnar motor study recording the contralateral first dorsal interosseous, stimulating the wrist (in order to compare distal latencies and amplitudes side to side)
10. Lumbrical–interossei distal latency comparison study
11. Ulnar motor study recording the first dorsal interosseous, inching across the wrist in 1 cm increments
The following patterns are consistent with ulnar neuropathy at the wrist:
DML to FDI: >4.5 ms (provided CMAP amplitude is not markedly reduced)
DML comparing FDI to ADM: >2.0 ms difference
DML comparing symptomatic FDI to contralateral FDI: >1.3 ms difference
DML comparing ulnar INT to second lumbrical: >0.4 ms difference
The following patterns denote ulnar neuropathy at the wrist with certainty:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









