Normal median nerve (arrows) in the middle of the forearm. Notice the honeycomb-like echotexture in the transversal (A) and the fascicular echotexture in the longitudinal (B) scan. FDS = flexor digitorum superficialis, FDP = flexor digitorum profundus, FCR = flexor carpi radialis.
Pathological findings
Compressive neuropathies
The compressive neuropathies, and in particular entrapment syndromes, represent the most common pathologic conditions of the nerves. NUS allows examination of the most frequent entrapment sites in the upper extremities, for example, the carpal tunnel (median nerve), the cubital tunnel and Guyon’s canal (ulnar nerve) and the supinator tunnel (interosseous posterior nerve). In the lower extremities, the peroneal nerve at the fibular head, the tibial nerve in the tarsal tunnel, the interdigital nerves (Morton’s metatarsalgia) and the lateral femoral cutaneous nerve can be examined.
The basic diagnostic criterion is the visualization of nerve compression, which appears regardless of anatomic location on longitudinal scans as an abrupt flattening (notching) at the site of nerve compression and a fusiform swelling proximal and distal to it (Figure 26.2). The swelling is accompanied, depending on the degree of compression, by hypoechogenicity and fogging or extinction of the typical fascicular echotexture resulting from nerve edema. Correspondingly, the transverse sections show an enlargement of the nerve cross-sectional area of a hypoechoic nerve. The sonographic findings thus reflect the pathomorphological changes in terms of nerve constriction at the site of compression and the pseudoneuroma formation seen intraoperatively. In addition, NUS allows evaluation of the surrounding structures and finding nerve compression etiology (e.g., compression by a mass lesion). Anatomical variations can be evaluated as well. Thus, NUS helps in planning and timing further therapy (conservative/operative, e.g., in case of compression by a mass lesion early surgical therapy is indicated).
Carpal tunnel syndrome
Carpal tunnel syndrome (CTS) is the most common peripheral nerve disorder with a lifetime prevalence of about 15%. In typical cases, the longitudinal scans show a nerve compression under the flexor retinaculum with the formation of a pseudoneuroma proximally and (often to a lesser extent) distally to the retinaculum. The transversal scans show a nerve enlargement at the site of pseudoneuroma, which is quantified by cross-sectional area measurements at the level of the carpal tunnel inlet (pisiform bone, cross-sectional area > 0,11 cm2). In rare cases, an enlargement at the carpal tunnel outlet only can be seen. NUS has a sensitivity (from 73% to 92%) and specificity comparable to electrophysiological methods [5]. Furthermore, NUS represents a complementary method to electrodiagnostic testing. Even with normal electrophysiology NUS can detect pathological findings, and vice versa.
An even more important contribution of NUS is to rule out secondary CTS that includes tenosynovitis of the flexor tendons, ganglia, arthrotic and arthritic conditions, amyloid deposits, accessory muscles or median artery thrombosis [6,7]. Furthermore, anatomical variants, such as prolonged muscle bellies of the finger flexors reaching into the tunnel, can be detected. More important are nerve variants such as bifid median nerve or variants of the thenar branch (subligamentary or transligamentary course). Also, vessel variants like a persisting median artery or atypical course of the ulnar artery can be seen. The detection of such variants can be significant especially for the endoscopic surgeon. In every third patient with CTS, sonography found one of the above-mentioned structural abnormalities [7].
NUS plays a very important role in postoperatively persisting or recurrent CTS. It allows visualization of surgically treatable causes like incomplete retinaculum transection, or surgery complications such as abnormal scarring, postoperative tenosynovitis or iatrogenic nerve injury. Based on personal experience, sonography can also find false preoperative diagnoses, discovering conditions mimicking CTS like nerve tumor [8] or neuritis.
Ulnar neuropathy at the elbow
Ulnar neuropathy in the elbow region (UNE) comprises three entities each with its own etiology and therapy. The cubital tunnel syndrome represents the most common disorder. In this condition the nerve compression takes place under the aponeurosis/ligament between the origins of the ulnar flexor muscle of the wrist (humeroulnar arcade, Osborne ligament). Correspondingly, ultrasound shows a flattening of the nerve under the arcade with a proximal swelling in the sulcus. Cross-sectional areas >0.1 cm2 accompanied by a hypoechoic appearance and loss of the honeycomb echotexture, are diagnostic for cubital tunnel syndrome.
Another entity is caused by repetitive dislocation of the nerve out of the sulcus leading to chronic pressure damage. A lacking or loose humeroulnar arcade is postulated as a reason for this. In the case of subluxation, the ulnar nerve is located at the tip of the medial epicondyle at maximum elbow flexion. In the case of luxation, it is dislocated volar to the medial epicondyle. The nerve dislocation is often accompanied by a nerve swelling [3].
Further, space-occupying lesions such as ganglia, lipomas, arthritic and arthrotic changes, accessory muscles or a dislocation of the medial triceps head (“snapping triceps syndrome”) can be reliably identified. In these cases, the compression is often located proximal to the cubital tunnel, which may result in atypical electrophysiological findings.
The diagnostic value of sonography is comparable with electrophysiological methods, in combination it improves the diagnostic yield. In addition, it provides prognostic information: the extent of swelling in the sulcus correlates negatively with clinical improvement after surgery [9].
Less common compression syndromes
Since the less common compression syndromes affect predominantly smaller nerves, the sonographic depiction of a direct nerve compression is more difficult. Therefore, the main role of sonography lies in the recognition of neighborhood processes as compression factors. NUS can detect space-occupying lesions such as ganglia or lipomas affecting the ulnar nerve in Guyon’s canal syndrome, the median nerve at the proximal forearm, the interosseous posterior nerve in the supinator tunnel, the axillary nerve in the quadrilateral space as well as the suprascapular nerve. In the so-called algetic posterior interosseous syndrome an ultrasound-guided infiltration can be performed for diagnostic purposes. In thoracic-outlet syndrome, sonography can reveal a compression of the spinal nerve C7 or C8 by cervical rib, fibrous bands [10] or bony processes.
In the lower extremities, the peroneal nerve at the fibular head and the tibial nerve in the tarsal tunnel can be compressed by different soft tissue masses (enlarged bursae, ganglia, heterotopic ossification after trauma). The peroneal nerve in particular can be affected by intraneural ganglia emerging from the tibiofibular joint via the articular branch [11].
In Morton’s metatarsalgia a “neuroma-like enlargement” of the second or third plantar interdigital nerves can be seen. Even in obese patients with meralgia paresthetica, a compression of the lateral femoral cutaneous nerve can be demonstrated and combined with an ultrasound-guided infiltration (author’s personal experience) [12].
Sonography of peripheral nerve tumors
Peripheral nerve tumors could be detected with ultrasound back in the 1980s. This was possible because of their size: large nerve tumors can be visualized even with older transducers with a low scanning frequency (around 7 MHz).
The two most common types of peripheral nerve tumors are schwannomas (neurinoma) and neurofibromas. Sonographically, both appear as well-defined, round masses with a hyperechoic rim, which are localized in the course of a peripheral nerve. Schwannomas are predominantly homogeneously hypoechoic and lie eccentric to the long nerve axis, in contrast to neurofibromas, which lie central. A neurofibroma’s echogenicity is higher and often focused in the center of the mass (the so-called target sign) [13]. Schwannomas show often a hypervascularization in color-coded examination, in neurofibromas no significant internal perfusion can be seen even in contrast-enhanced ultrasound [14]. In so-called ancient Schwannomas, anechoic necrotic areas and a massive hypervascularization can be seen. Plexiform neurofibromas, which occur typically in neurofibromatosis type 1 (von Recklinghausen’s disease), spread over long segments of one or more nerves. The nerves are infiltrated with small nodules which form a dysmorphic mass of heterogeneous echogenicity uplifting the inner nerve architecture (“sack full of worms”) [15]. Perineuriomas are seldom seen, but may appear in young patients with painless, slowly progressive motor deficits. With NUS they appear as fusiform hypoechogenic structures without vascularization spreading over several centimeters (Figure 26.3).
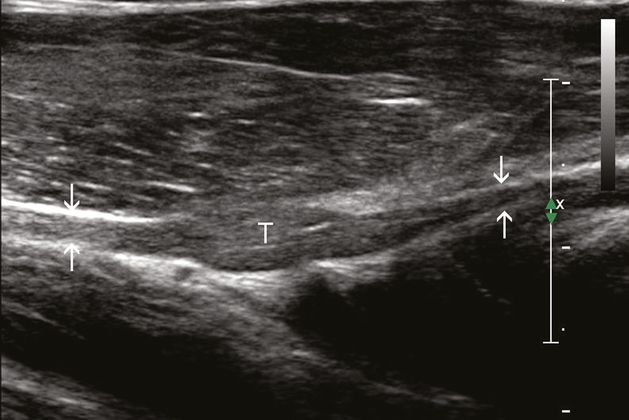
Perineuroma (T) of the posterior interosseous nerve (arrows) at the proximal forearm just before the entrance to the supinator tunnel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








