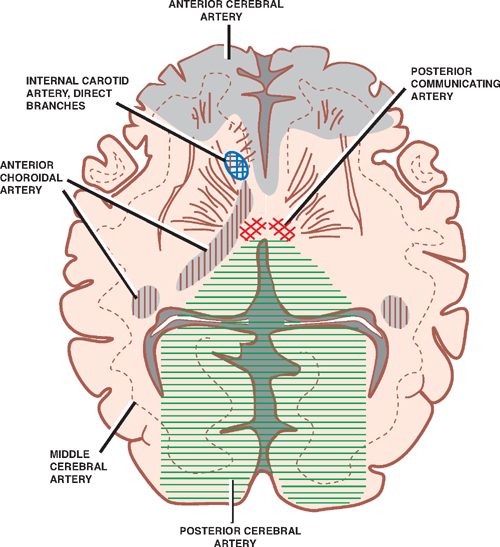
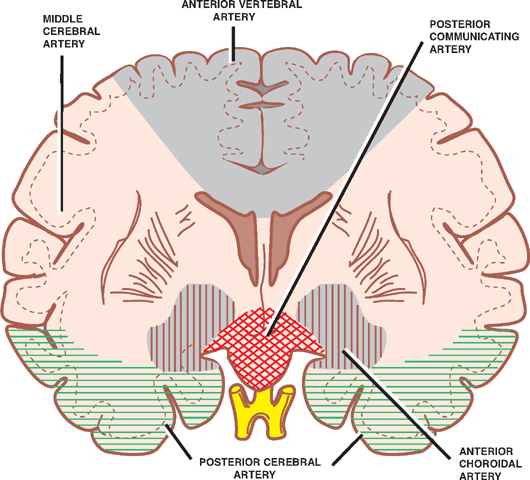
22 Vascular System Cerebrovascular diseases are one of the most common neurologic disorders, accounting for nearly 50% of all neurologic patients in a general hospital. Furthermore, stroke is the third leading cause of death among Americans. The clinical manifestation of a cerebrovascular lesion is marked by the sudden onset of a neurologic deficit and is termed a cerebrovascular accident or stroke. Two types of stroke are distinguished by their pathophysi-ological mechanisms: ischemic stroke (infarct), which is caused by hypoperfusion, thrombosis, or embolism, and hemorrhagic stroke, which is caused by intracranial bleeding. The often devastating effect of stroke, or cerebral infarction, is in part explained by the fact that neural tissue is so exquisitely sensitive to an interruption in blood flow: brain dysfunction occurs within 8 to 10 seconds of interrupted perfusion, and by 3 to 5 minutes brain damage is permanent. This occurs because the brain is completely reliant on blood flow to provide metabolic substrates (e.g., glucose) and oxygen. Although the brain constitutes only 2% of the body weight, it requires roughly 17% of the cardiac output and consumes ~20% of the oxygen that is utilized by the body. Due to this high demand and reliance on perfusion for energy production, the brain has developed a system of autoregulation. Autoregulation is the capacity of the brain to maintain cerebral blood flow in the face of systemic hypotension. Autoregulation is primarily determined by metabolic needs but is also increased by systemic blood pressure. For example, both carbon dioxide accumulation and low blood pressure result in cerebral vasodilatation. Therefore, despite the systemic blood pressure (within a specific range of 60 to 160 mm Hg), the brain receives a constant perfusion and energy supply. Fig. 22.1 Blood supply of the brain, axial view. See Figs. 22.1, 22.2, 22.3, and 22.4 and Table 22.1. The arteries of the brain are divided into two systems named after their branches of origin: the internal carotid system and the vertebrobasilar system. An anastomotic connection between these two systems, the circle of Willis, provides a clinically important collateral supply (see later discussion). The internal carotid system, also known as the anterior circulation, comprises the internal carotid artery and its terminal branches, the anterior and middle cerebral arteries. Prior to its terminal bifurcation, the (intradural, supraclinoid) internal carotid artery gives rise to the ophthalmic, the posterior communicating, and the anterior choroidal arteries, in that order. Fig. 22.2 Blood supply of the brain, coronal view. The vertebrobasilar system, also known as the posterior circulation, comprises the vertebral and basilar arteries. Branches of the vertebral arteries include the menin-geal artery, the anterior and posterior spinal arteries, and the posterior inferior cerebellar artery. Branches of the basilar artery include the anteroinferior cerebellar artery, the labyrinthine artery, the pontine arteries, the superior cerebellar artery, and its terminal branch, the posterior cerebral artery. This system supplies the medial and inferior aspects of the occipital and temporal lobes, the thalamus, the brainstem, the cerebellum, and the upper spinal cord.
The Blood Supply of the Brain
| Internal Carotid | Vertebral | Basilar |
| Ophthalmic | Meningeal | Anteroinferior cerebellar |
| Posterior communicating | Posterior spinal | Labyrinthine |
| Anterior choroidal | Anterior spinal | Pontine |
| Anterior cerebral | Posteroinferior cerebellar | Superior cerebellar |
| Middle cerebral | Posterior cerebral |
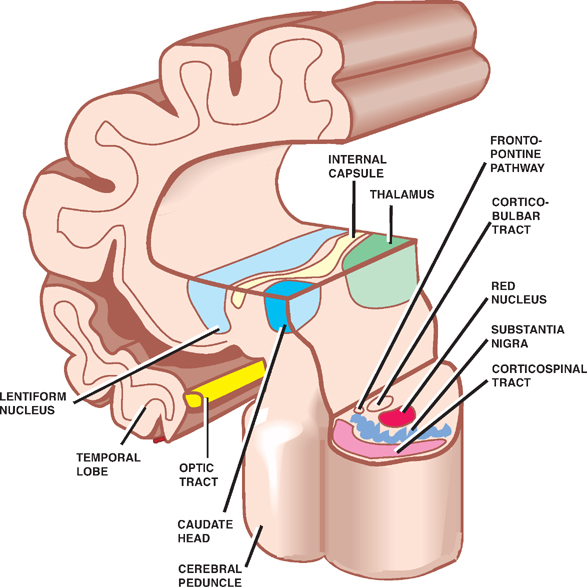
Fig. 22.3 Anatomy of internal capsule, basal ganglia, and cerebral peduncle.
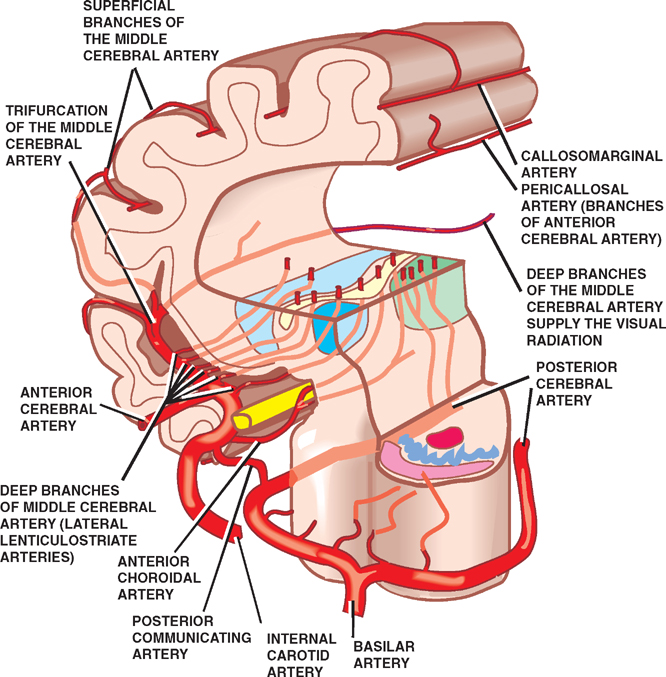
Fig. 22.4 Blood supply of the deep structures of the hemisphere.
The Internal Carotid System
See Figs. 22.5, 22.6, and 22.7.
The internal carotid system supplies the anterior two thirds of the brain.
The internal carotid artery (ICA) arises from the bifurcation of the common carotid artery. From its origin in the neck to its termination in the cerebrum, the ICA (1) enters the cranial cavity by passing through the carotid canal; (2) travels through the cavernous sinus next to the oculomotor nerve (III), the trochlear nerve (IV), the ophthalmic and maxillary divisions of the trigeminal nerve (VI and V2), and the abducens nerve (VI); (3) penetrates the dura and the arachnoid mater to enter the subarachnoid space; and (4) divides into terminal branches at the medial end of the lateral cerebral sulcus (sylvian fissure).
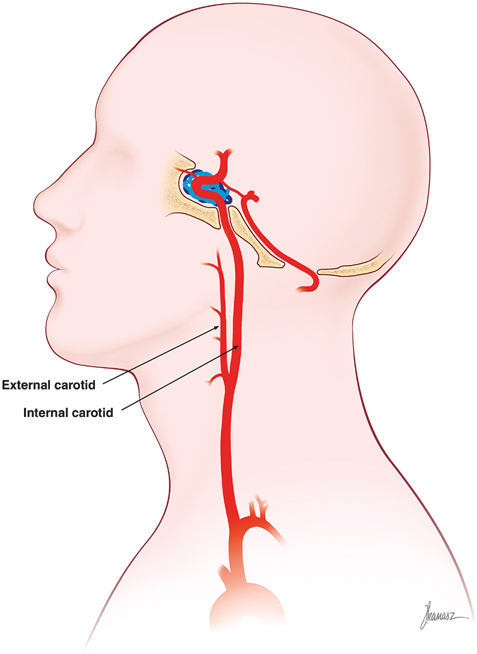
Fig. 22.5 Internal carotid artery.
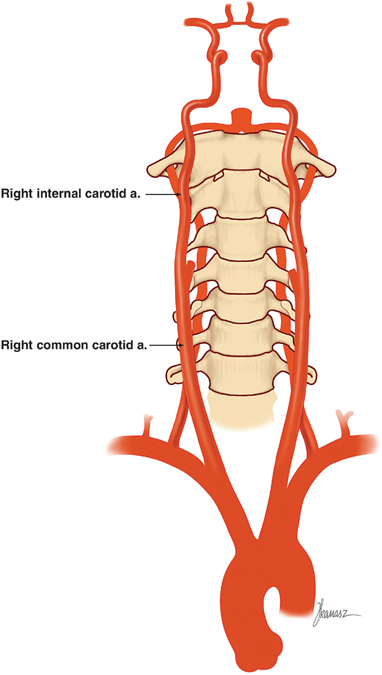
Fig. 22.6 Internal carotid and vertebral artery systems.
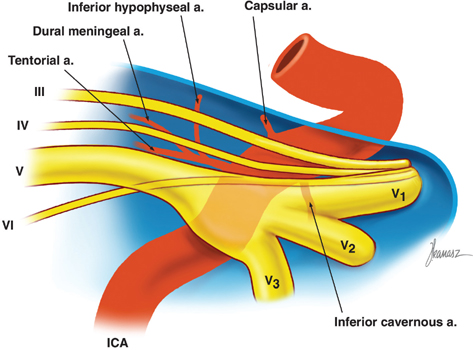
Fig. 22.7 Internal carotid artery, cavernous sinus portion.
The Five Major Branches of the Internal Carotid Artery
- The ophthalmic artery (Fig. 22.8) takes its origin as the ICA emerges from the cavernous sinus to enter the subarachnoid space. It passes through the optic canal and into the orbit, inferolateral in relation to the optic nerve. Its major branch is the central retinal artery, which travels in the optic nerve and supplies the neuroretina. The ophthalmic artery forms clinically important anastomoses with branches of the external carotid artery, effectively connecting the internal and external carotid arteries. Occlusion of the ophthalmic artery may cause monocular blindness in the ipsilateral eye.
- The posterior communicating artery (Fig. 22.9) arises from the inferolateral wall of the ICA near the terminal bifurcation of the ICA. It courses posteriorly above the third nerve to anastomose with the proximal portion of the posterior cerebral artery, forming part of the circle of Willis. Many perforators emerge from this artery that supply the posterior hypothalamus, anterior thalamus, posterior limb of the internal capsule, and subthalamus.
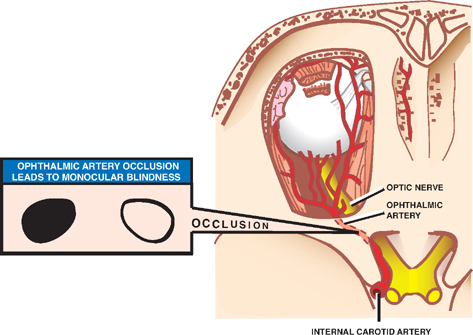
Fig. 22.8 Ophthalmic artery.
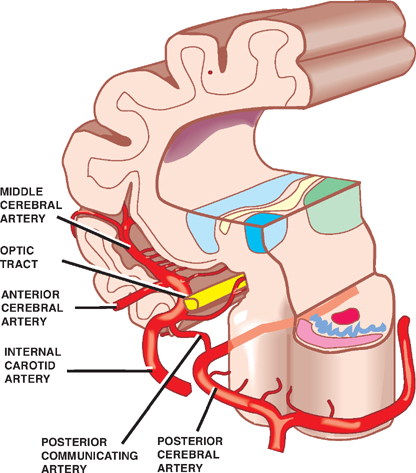
Fig. 22.9 Posterior communicating artery.
- The anterior choroidal artery (Figs. 22.10, 22.11, and 22.12) arises just distal to the posterior communicating artery, also near the terminal bifurcation of the ICA. It passes dorsally along the optic tract at the medial edge of the temporal lobe, where it enters the choroidal fis-sure and angiographically this is known as the plexal point. It terminates in the temporal horn of the lateral ventricle, where it supplies the choroid plexus. Along its course it gives small branches to surrounding subcortical structures, including the optic tract, the lateral geniculate body, the lentiform nucleus, the thalamus, the hippocampus, and the internal capsule (genu and posterior limb).
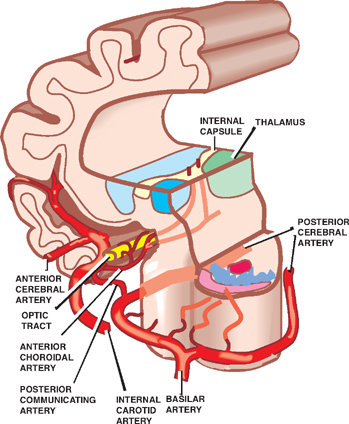
Fig. 22.10 Anterior choroidal artery, coronal view.
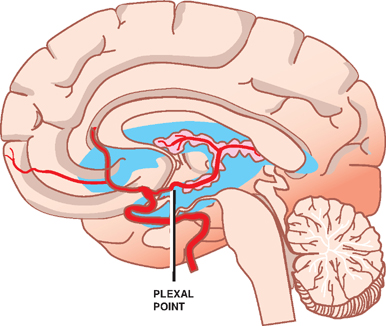
Fig. 22.11 Anterior choroidal artery, sagittal view.
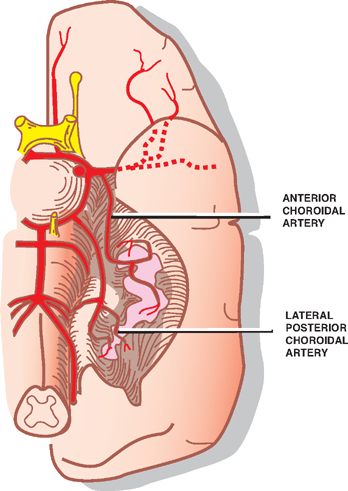
Fig. 22.12 Anterior choroidal artery, axial view.
- The anterior cerebral artery (ACA) (Figs. 22.13, 22.14, and 22.15) is the smaller of the two terminal branches of the ICA. It runs forward and medially above the optic nerve. Before it enters the interhemispheric fissure, it is joined to the ACA of the opposite side by the anterior communicating artery. This is also an important aspect of the circle of Willis. The artery then enters the fissure and courses upward and backward on the medial surface of the hemisphere, along the superior aspect of the corpus callosum. The cortical branches of the ACA supply the medial aspect of the frontal and parietal lobes, including the leg area of the pre- and postcentral gyri. The central branches of the ACA (recurrent artery of Heubner or medial striate artery) penetrate the anterior perforated substance to supply the anteromedial parts of the basal ganglia and anterior limb of the internal capsule.
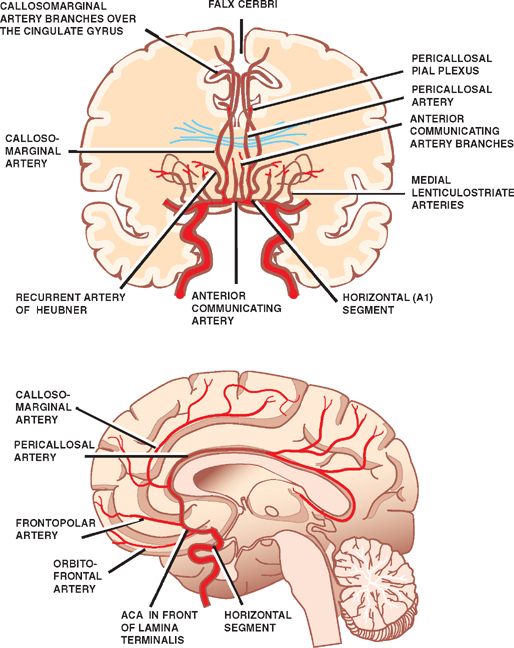
Fig. 22.13 Anterior cerebral artery and its branches.
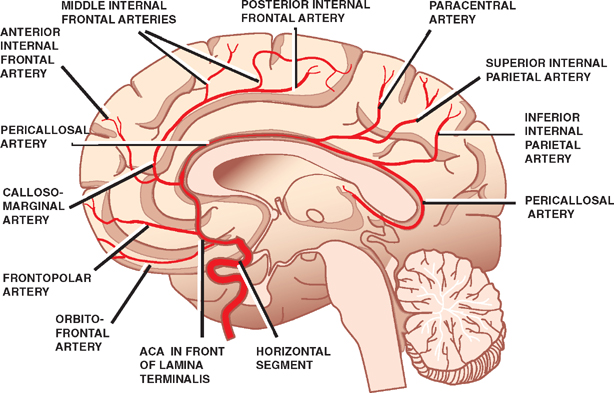
Fig. 22.14 Anterior cerebral artery and its branches.
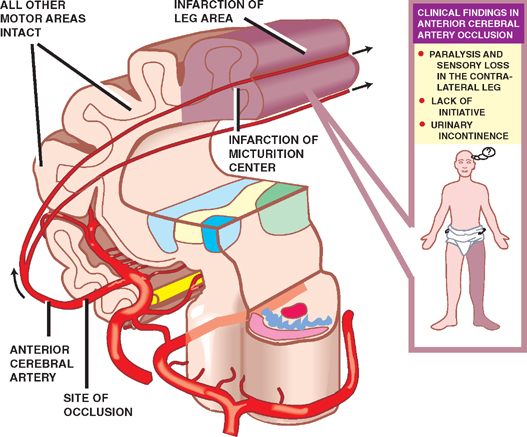
Fig. 22.15 Anterior cerebral artery occlusion.
- The middle cerebral artery (MCA) (Fig. 22.16) is the largest of the two terminal branches of the ICA and is considered to be its direct continuation. The artery runs laterally in the lateral cerebral sulcus, where it divides into cortical and central branches.
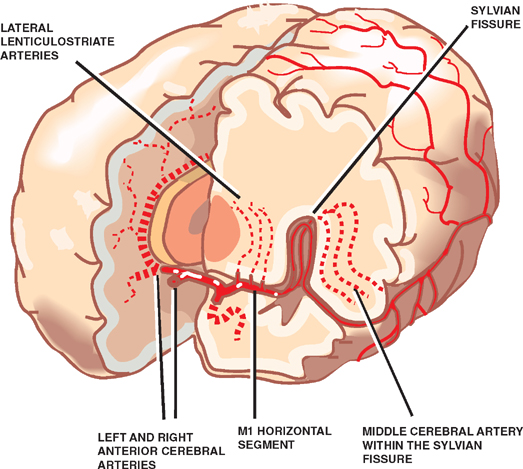
Fig. 22.16 Middle cerebral artery.
The cortical branches of the MCA supply most of the cortex on the lateral side of the hemisphere (Fig. 22.4). A superior division supplies the motor and sensory cortex related to the face and arm and the area of expressive language (Broca’s area) of the dominant hemisphere. An inferior division supplies part of the optic tract, the upper part of the optic radiations, and the area of receptive language (Wernicke’s area) of the dominant hemisphere. The central branches of the MCA (lenticulostriate arteries) penetrate the anterior perforated substance and supply most of the basal ganglia and internal capsule (Fig. 22.5).
Vascular Syndromes Associated with Five Major Internal Carotid Artery Branches
Occlusion of the MCA (or one of its divisions) is the most common cause of ischemic stroke. The vascular syndrome produced depends on the division (or divisions) involved (Fig. 20.4, p. 493).
Occlusion of the superior division (Fig. 22.17) produces (1) contralateral paralysis of the face and arm due to involvement of the motor cortex, (2) contralateral sensory loss of the face and arm due to involvement of the sensory cortex, and (3) Broca’s (expressive) aphasia (dominant hemisphere) due to involvement of the inferior frontal gyrus.
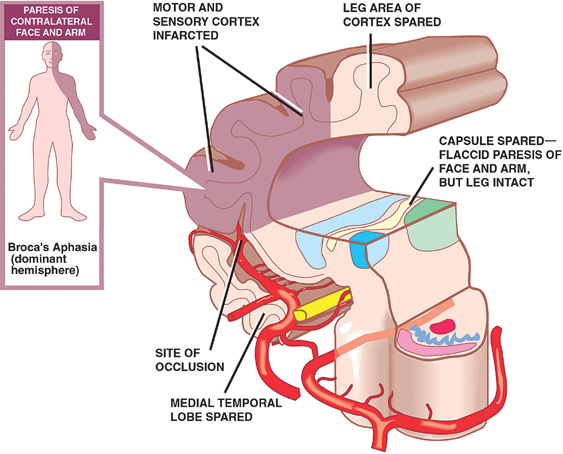
Fig. 22.17 Superior division occlusion.
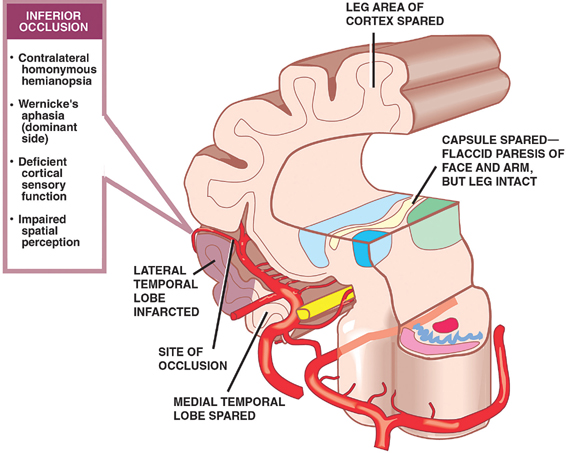
Pure inferior division (Fig. 22.18) stroke is a less frequent event. It produces (1) contralateral homonymous hemianopsia due to interruption of the optic tract or radiations; (2) Wernicke’s (receptive) aphasia (dominant hemisphere) due to involvement of the posterior superior temporal gyrus; (3) deficient cortical sensory function (e.g., inability to discriminate the form of an object by touch) due to involvement of the primary, secondary, or association sensory cortex; and (4) impaired spatial perception (e.g., lack of awareness of neurologic deficit, and neglect of contralateral limbs and space) due to involvement of the nondominant parietal lobe.
Occlusion of a central branch of the MCA causes contralateral paralysis involving the face, arm, and leg due to involvement of the internal capsule.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








