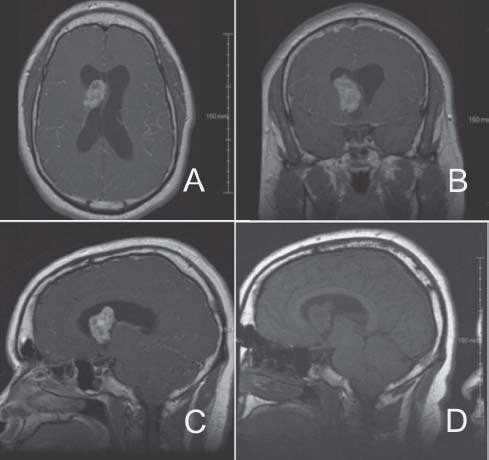
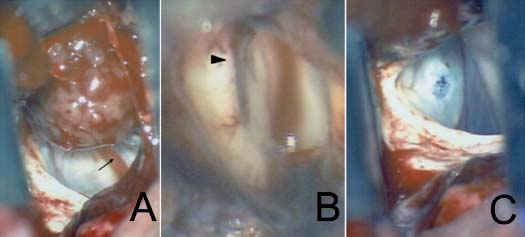
Case 2 Subependymal Giant Cell Astrocytoma Fig. 2.1 Magnetic resonance imaging (MRI) scan of the brain (A–C) with gadolinium intravenous contrast and (D) without contrast showing (A) pertinent axial, (B) coronal, and (C,D) sagittal sections. Fig. 2.3 Intraoperative pictures taken with microscope magnification (300×) showing the inside of the right lateral ventricle (A) with large fleshy mass superiorly representing the tumor. A small draining vein within the ventricle is pointed out (arrow). Following tumor resection, the picture is taken while inside the lateral ventricle showing the slitlike opening (arrowhead) into the third ventricle via the foramen of Monro (B). Picture taken while retracting with a self-retaining retractor and exposing the medial wall of the lateral ventricle (C).
 Clinical Presentation
Clinical Presentation
 Questions
Questions
< div class='tao-gold-member'>
2 Subependymal Giant Cell Astrocytoma
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree


