Case 3 Sturge–Weber Syndrome
Remi Nader
Fig. 3.1 (A,B) Computed tomography scan without contrast, brain windows, and bone windows (C,D), showing lesion in the left hemisphere.
- A 31-year-old man had a grand mal seizure episode at home while eating.
- He is brought to the emergency room at an outside hospital, where he obtains a computed tomography (CT) scan, which is read as “suspicious subarachnoid hemorrhage.” He is then transferred to your hospital for further care. On arrival, the patient was in status epilepticus, intubated, and receiving diazepam and phenytoin.
- Initial CT scan is shown in Fig. 3.1.
- The family arrives shortly after patient is stabilized and further history is obtained.
- The patient is known to have a seizure disorder, and the first seizure was 6 years ago. He also has a longstanding expressive speech deficit. He has had a left-sided hemiparesis for the past 6 years with joint contractures.
- The family was told by his primary care physician that he has a “brain condition” for which they did not know the name.
- He recovers back to his baseline neurologic status the next day.
Fig. 3.2 (A,B) Magnetic resonance images with contrast, (C) magnetic resonance angiography coronal, and (D) axial reconstructed images showing abnormality in the left hemisphere.
< div class='tao-gold-member'>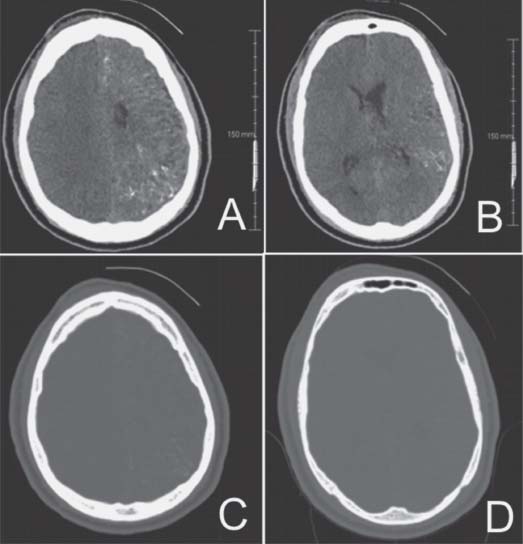
 Clinical Presentation
Clinical Presentation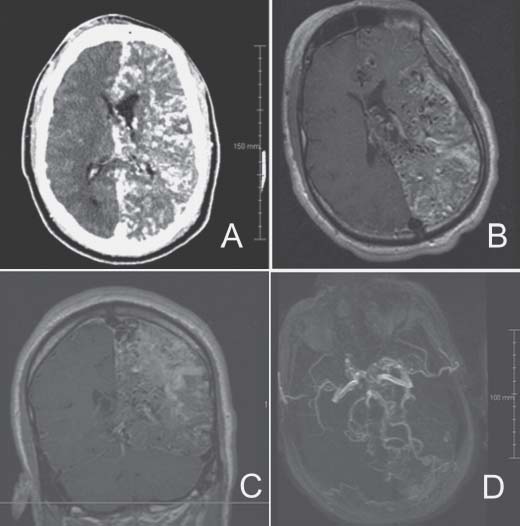
 Questions
Questions Answers
Answers


