Case 6 Olfactory Groove Meningioma
Stephen J. Hentschel and Lissa Marie Ogieglo
Fig. 6.1 Axial computed tomography (CT) scan of the brain plus contrast.
- A 78-year-old woman presented with increasing difficulties with ambulation and memory deficits. The patient also complained of progressive visual loss for an unspecified period.
- Medical history is significant for atrial fibrillation and hypothyroidism treated with Eltroxin (GlaxoSmithKline, Brentford, London, UK), digoxin, and warfarin.
- On examination, the patient was confused and agitated. She had a right temporal visual field cut and decreased acuity in the left eye. Her examination was otherwise unremarkable but difficult to assess because of her confusion.
- A computed tomography (CT) scan of the head was performed (Fig. 6.1). The patient was then admitted for further management.
Fig. 6.2 (A) Axial T1-weighted magnetic resonance image (MRI) plus gadolinium of the brain. (B) Sagittal T1-weighted MRI plus gadolinium of the brain.
< div class='tao-gold-member'>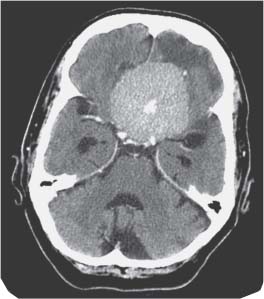
 Clinical Presentation
Clinical Presentation Questions
Questions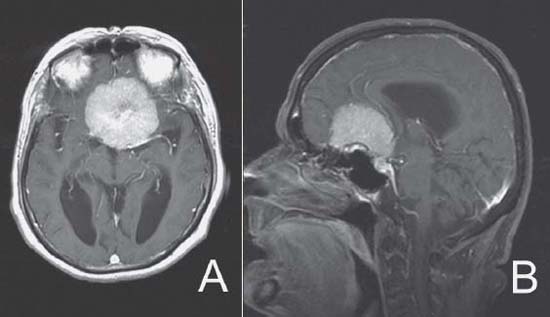
 Answers
Answers


