Case 7 Sphenoid Wing Meningioma
Remi Nader
Fig. 7.1 T1-weighted magnetic resonance imaging sequences with contrast illustrating sphenoid wing meningioma. (A) Axial, (B) sagittal, and (C,D) coronal sections of interest are shown.
- A 53-year-old woman presents with a history of chronic headaches on the right side for several years with more recent exacerbation.
- She reports a history of partial seizures for the past 9 months.
- The patient has a long history of left-sided decreased sensation along her face, arm, and lower extremity, as well as some subjective weakness along her left side. She claims that these symptoms have been present since she sustained a stroke about a year ago.
- She also complains of some right-sided blurred vision and decreased visual acuity along the right eye.
- She has some gait disturbances.
- She is referred with magnetic resonance imaging (MRI) (Fig. 7.1). You are told that the lesion observed was present 5 years ago but was about half its current size.
< div class='tao-gold-member'>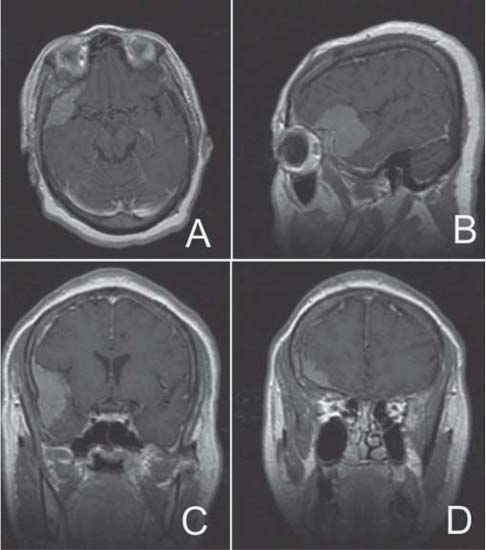
 Clinical Presentation
Clinical Presentation Questions
Questions Answers
Answers


