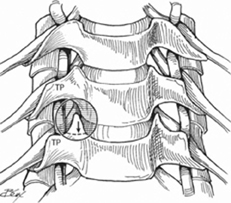
15 Neil R. Malhotra and M. Sean Grady Anterior cervical foraminotomy is performed when there are isolated one-level radicular symptoms without findings to support the need for complete diskectomy. In contrast to posterior foraminotomy, the anterior approach provides access to anterior osteophytes and free disk fragments with minimal nerve manipulation. Cervical foraminotomy performed from an anterior approach permits removal of offending spondylotic bone spur or compressive extranuclear disk material in combination with direct visualization of the nerve root. Cervical foraminotomy can significantly improve disability that has resulted from neural compression due to osteophyte formation and disk herniation. When radiculopathy is the primary presenting symptom, foraminotomy can result in significant reduction in radiculopathic symptoms. Although cervical diskectomy effectively addresses myelopathy, it is foraminotomy, with clear decompression of the nerve root, that most effectively addresses unilateral upper extremity radiculopathy. Failure to address foraminal free disk fragments and osteophytes will plague the patient and surgeon alike. The key pathology can be accessed and removed via foraminal exploration. Decompression of the nerve root leads to excellent outcomes in the appropriately selected patient population. Always counsel the patient about the risk of postoperative sympathetic plexus injury and Horner-type syndrome, as well as hoarseness, cerebrospinal fluid leak, and swallowing difficulties. Isolated unilateral radiculopathy, in conjunction with imaging that supports the finding of a free disk fragment, indicates the need for, and potential benefit of, anterior cervical foraminotomy. Anterior cervical foraminotomy is contraindicated in patients with neck pain and myelopathy. In myelo-pathic patients anterior cervical diskectomy and fusion is appropriate with appropriate pathology. Additionally, in the setting of posterior compression, or significant spondylolisthesis at adjoining levels, anterior foraminotomy is contraindicated. Preoperative imaging, including magnetic resonance imaging (MRI), and possibly plain x-ray, in conjunction with attention to the physical exam and a description of the location of pain permits tailoring of surgery to most benefit the patient. Perform flexion extension x-ray if a question of instability exists. Consider computed tomography (CT) scan through surgical levels if other imaging does not adequately resolve questions concerning bony pathology. The patient is placed supine on the operative table with a gel roll under the scapulae to aid extension and exposure of the operative field. A foam doughnut or horseshoe headrest placed under the head enables maximal safe extension and minimizes jaw intrusion into the operative field. Perioperative antibiotics should be administered 30 minutes prior to the skin incision. Fiberoptic intubation is generally not needed. Anesthesia colleagues should minimize the use of airway monitors such as temperature probe when alternative options exist. Shoulders should be taped down to maximize cervical exposure and permit adequate cross-table lateral x-ray to be taken for localization. Arms should be tucked at the patient’s side. Intraoperative physiologic monitoring is not needed.
Anterior Cervical Foraminotomy Technique
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned Dealing with Difficulties Encountered
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







