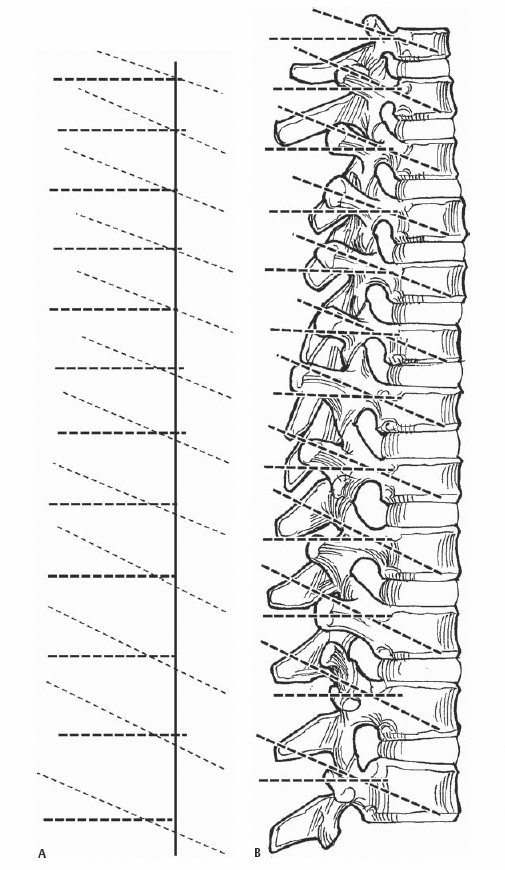
29 Timothy R. Kuklo Thoracic pedicle screws have become increasingly common for the treatment of spinal deformity, trauma, and tumors due to their superior fixation and improved correction. Theoretic concerns of increased neurologic complications from thoracic pedicle screw placement have not been proven. Maximizing pedicle screw and construct advantages requires an understanding of pedicle screw biomechanics, including screw characteristics and insertion techniques. In addition, an understanding of bone quality, pedicle morphometry, and screw salvage options is necessary. This is best illustrated by the fact that the pedicle, rather than the vertebral body, contributes approximately 80% of the stiffness and approximately 60% of the pullout strength at the screw-bone interface. The major screw design variables include thread pitch, shaft design, inner (minor) and outer (major) diameter, head size and design, and material composition. In general, the most important variable to improve thoracic pedicle screw fixation is the outer diameter, whereas the inner to outer diameter ratio (ID/OD) has a smaller effect. Increasing pitch (more threads per inch) has only a minor effect. Approximately 75% of the pullout strength is achieved by crossing the neurocentral junction, or physeal scar, whereas anterior cortical purchase has a small additional effect on pullout, but is generally not recommended due to potential complications. Engagement of 50 to 80% of the vertebral body on a lateral radiograph appears optimal. Intrapedicular thoracic pedicle screw placement is superior to an extrapedicular (in-out-in) placement, which achieves only 64% of the pullout strength compared with intrapedicular placement. Further, a straightforward trajectory (directing the pedicle screw parallel to the superior vertebral end plate) is biomechanically superior to an anatomic trajectory (directing the pedicle screw along the sagittal anatomic pedicle axis approximately 20 to 25 degrees caudad) (Fig. 29.1). However, if a straightforward trajectory is not achieved due to pedicle wall violation or some other condition, then a salvage strategy using the anatomic trajectory will again achieve 60 to 70% of the pullout strength compared with the ideal straightforward trajectory. Fig. 29.1 (A) Lateral schematic of straightforward and anatomic trajectories. (B) Lateral image of thoracic pedicle screw placement utilizing the straightforward and anatomic trajectory techniques. When performing construct testing, pedicle screw constructs again provide improved construct stiffness; however, lateral pullout is the weakest testing mode for thoracic pedicle screws. Cross-links improve construct torsional stability when using thoracic pedicle screws. Spinal deformity, trauma or tumors, especially with destabilizing procedures such as vertebral osteotomies, resection, or correction. Inadequate-sized or compromised pedicles. A thorough understanding of surgical anatomy is paramount to successful thoracic pedicle screw placement. As recently as several years ago, the thoracic pedicle was thought to be a rather homogeneous, ovoid structure throughout the thoracic spine. However, we now know that the anatomy of the pedicle is quite complex and varies from region to region in the thoracic spine. Pedicle height, or sagittal pedicle isthmus width, varies from 12.0 to 20.0 mm (mean 15.8 mm) at T12 to 7.0 to 14.5 mm (mean 9.9 mm) at T1, and is never the limiting factor. Pedicle width is the critical anatomic variable. In the adult lower thoracic spine (T10–T12), the average pedicle width averages from 6.3 to 7.8 mm, often larger than the average pedicle width at L1 and L2. Pedicle width then decreases with a more cephalad vertebral level, and is usually the smallest at T4–T6. The interpedicular distance, or canal width, is also widest in the lower thoracic spine and subsequently decreases more cephalad until approximately T4, where it is often the narrowest. Thus T4 may be one of the most difficult thoracic pedicle screws to place, especially with a coronal deformity. The coronal or transverse pedicle axis varies from cephalad to caudad, with the greatest transverse angle being at T1. Clinically, pedicle screw insertion depends on this axis, as well as the preferred start point (Fig. 29.2). The sagittal pedicle axis has received less attention, with the pedicle inclination routinely averaging between 20 and 25 degrees throughout the thoracic spine, with only small differences between males and females. The medial wall is also between two and three times thicker than the lateral wall throughout all thoracic levels.
Thoracic Pedicle Screw Placement: Anatomic, Straightforward, and In-Out-In Techniques
Description
Key Principles
Indications
Contraindications
Special Considerations

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








