32
Anterior Thoracic Arthrodesis Following Corpectomy (Expandable Cage, Metallic Mesh Cages)
D. Greg Anderson and Chadi Tannoury
Description
Various spine pathologies, such as fractures, destructive infections, and tumors, affect the vertebral body and lead to spinal instability. Surgical restoration of the anterior column, using metallic meshes or expandable cages, aims to decompress neural elements and provide biomechanical stabilization of the thoracolumbar spine following vertebrectomy.
Key Principles
The use of autogenous tricortical iliac bone graft for vertebral body replacement has been a standard technique for vertebral body replacement in the past. However, problems with this approach including donor-site morbidities, pseudarthrosis, graft displacement, and graft collapse with kyphotic deformity have been reported. In recent years, a variety of surgical implants (cages) have been manufactured for vertebral body replacement in the thoracolumbar spine. First-generation cages for this purpose were made from titanium mesh or carbon fiber reinforced PEEK materials. More recently, complex cage designs have proliferated, including some cages that are “expandable,” allowing the surgeon to place the cage into the spinal defect and lengthen or expand the cage to fill the defect or eliminate residual kyphosis at the corpectomy site (Fig. 32.1). Expandable cages offer several surgical advantages over nonexpandable metallic meshes; expandable implants can be inserted at a small volume through minimally invasive incisions, and the adaptation of the implant configuration to the exact defect height is possible by in vivo extension of the device, thereby avoiding further trimming of the nonexpendable cages. In general, cages are designed to support bone in-growth or facilitate fusion across the corpectomy site.
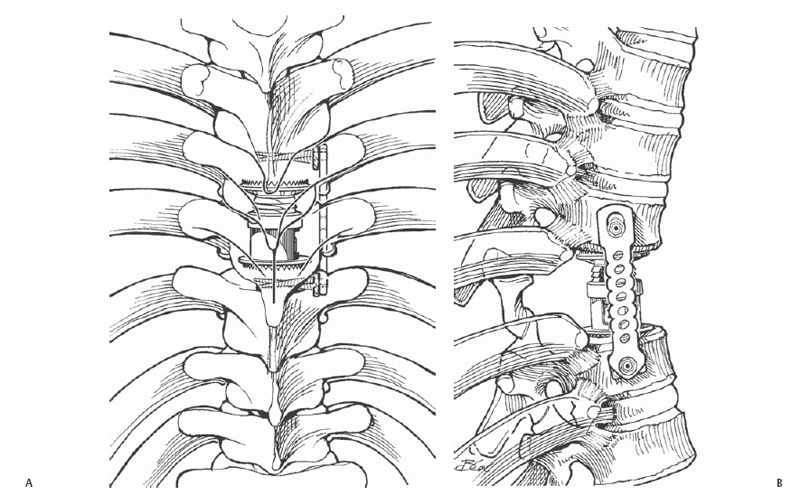
Fig. 32.1 (A) Anterior-posterior illustration of a thoracic arthrodesis construct using an expandable cage and a posterior instrumentation following corpectomy in a trauma patient. (B) Lateral illustration of a thoracic arthrodesis construct using an expandable cage and anterior instrumentation following corpectomy in a trauma patient.
Expectations
The use of a corpectomy cage is expected to reconstruct the anterior column of the thoracolumbar spine, restore normal alignment, provide stabilization, and achieve a solid fusion across the spinal defect. Clinically, this approach is designed to repair the spinal defect and provide a long-term stable solution to the underlying spinal disorder.
Indications
Vertebral body replacement is indicated in various pathologic conditions affecting the anterior column integrity, including certain fractures, tumors, destructive lesions, infections, and deformities.
Contraindications
Anterior column reconstruction should not be attempted as a primary or stand-alone treatment for severe spinal injuries with translation of the spine or rigid spinal deformities. Great care should be taken when anterior column bone quality is poor due to the risk of implant failure or subsidence. Also, many authors recommend avoiding prosthetic spinal implants in the settings of an active pyogenic infection.
Special Considerations
To promote bone in-growth into and through the cage implant, bone graft or a bone substitute should be used. Depending on the clinical scenario, autogenous bone from the corpectomy site, morselized rib graft, iliac crest graft, allograft bone, ceramic bone substitutes, or even purified bone proteins have been used.
Special Instructions, Position, and Anesthesia
The thoracic and thoracolumbar spine is approached with the patient placed in a lateral decubitus position. The ipsilateral lung may be deflated using double-lumen endotracheal tube ventilation, or ventilation pressures may be decreased allowing visualization of the spine. It is helpful to use neurophysiologic monitoring of the status of the neural elements, depending on the clinical scenario.
Tips, Pearls, and Lessons Learned
A preoperative identification of the diseased vertebra is crucial prior to surgery. In cases where the vertebral abnormality is not clearly evident on plain films, a sagittal magnetic resonance imaging (MRI) that includes the lumbosacral junction and the lesion on the same film is useful, so that the operating surgeon can count the levels up from the sacrum to the lesion using fluoroscopy. A metallic marker placed over the spine may be used to identify the proper location for the skin incision prior to starting. Before starting the corpectomy, the rib heads should be removed to allow identification of the pedicle and posterior corner of the vertebral body. A wide exposure of the involved vertebrae is beneficial to ensure proper alignment of the implant following the corpectomy. Anterior exposure of the vertebra is facilitated by packing small sponges along the anterior aspect of the spine to retract the adjacent blood vessels. Maintenance of the bony end plates of the adjacent vertebrae is important to seat the cage and diminish the odds of subsidence of the cage.
Difficulties Encountered
Poor localization of the incision or thoracotomy can make proper performance of the corpectomy and alignment of the cage difficult. Bleeding from the corpectomy or epidural vessels should be controlled with hemostatic agents. Ensure proper selection of cage length with the spine in a corrected position by manually applying force to the apex of the kyphotic deformity (push over the spine). This generally reduces the kyphosis at the corpectomy site and prevents undersizing of the cage implant.
Key Procedural Steps
Approach
A thoracotomy or thoracoabdominal approach is performed in the lateral decubitus position. Segmental vessels are ligated and divided as needed to facilitate the procedure. Three to four cm of rib head are removed at the level of the corpectomy to expose the underlying pedicle and posterior region of the vertebral body. The exiting nerve root is protected during the procedure.
Corpectomy
A Kerrison rongeur is first used to remove the pedicle and expose the lateral aspect of the spinal cord. A diskectomy of the adjacent intervertebral disks is then performed. The end plates of the adjacent vertebral bodies are carefully preserved to provide a solid support for the intervertebral cage implant. The anterior portion of the vertebral body is then removed with a rongeur or osteotome. The posterior wall of the vertebral body can be thinned with a high-speed burr and pushed away from the spinal cord with a small angled curette. The posterior longitudinal ligament can be removed to visualize the dura if indicated. In cases without infection or tumor, the bone from the corpectomy site is saved to use as graft to pack in and around the cage implant.
Implant Placement
Nonexpandable Cages
Any deformity is manually corrected and the defect length is measured. An appropriate cage is selected and packed with bone graft or an appropriate substitute. The corpectomy site is distracted and gentle impaction of the cage is performed. If an expandable cage is chosen, the cage may be introduced into the defect in a collapsed state and lengthened to apply distraction to the spine at the corpectomy site (Fig. 32.1).
Concerns
Ensure that proper placement of the cage is achieved with radiographs or fluoroscopy prior to the completion of the procedure.
Bailout, Rescue, Salvage Procedures
If proper cage sizes are not available, use of either allograft bone (e.g., humerus, tibia, femur) or autogenous bone can be considered. If a stable anterior-only construct is not achievable, supplemental posterior instrumentation should be applied.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







