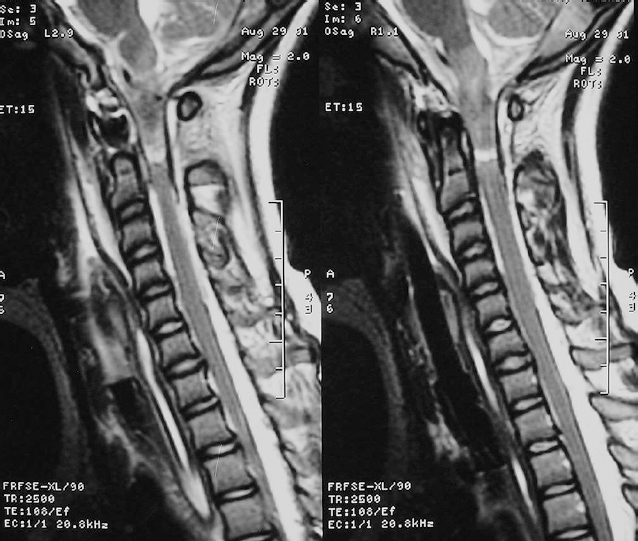
19 Biomechanical Considerations for Early Operative Interventions in Vertebral Column Fractures and Dislocations Melissa Y. Macias and Christopher E. Wolfla Approximately 160,000 new traumatic vertebral column injuries occur per year in the United States, 10% to 30% with concomitant spinal cord injury (SCI).1 An estimated 225,000 to 288,000 individuals currently live with SCI; the most common neurological level is cervical (51%) followed by thoracic (34.3%) and lumbosacral (10.7%). Accordingly, in the adult population, the cervical C4-C6 and thoracolumbar T12-L1 regions are the most frequently fractured or injured, 39.4% and 11.6%, respectively.1 Motor vehicle crashes (MVCs), particularly in the absence of occupant restraints, account for the majority of spine and spinal cord trauma. Less common causes are falls, acts of violence (most commonly gunshot wounds), and recreational sporting activities such as diving and contact sports. Since 2000, the proportion of SCIs due to sport-related activities and acts of violence have decreased, whereas those due to falls have increased. The average age at injury has steadily increased over time and is currently 37.6 years, likely reflecting the increase in the median age of the general population of the United States since the mid-1970s.1 Further, SCI in persons older than 60 has doubled since the 1980s, plausibly reflecting the concomitant increase in fall-related injuries in this population. Indeed, the cause of injury stratifies by age group with motor vehicle accidents, violence, and sport related-injuries more common in younger persons and falls more common in the elderly.1 Among adults, vertebral column fractures and fracture dislocations are the most common injury types. Most often, the degree of associated neurological injury correlates with the extent of vertebral column fracture and with associated dislocation or subluxation.2,3 In both adults and children, the cervical spine is the most frequently injured region of the spinal column following high-velocity or blunt trauma and is estimated to be 2% to 4% of all trauma patients.2,4 Accordingly, these injuries may be associated with neurological impairment. Though lower cervical injuries are common in both adult and pediatric population, atlanto-occipital dislocation is more prevalent in the pediatric age group.2,5 For all vertebral column injuries, initial management is focused on basic emergency and trauma management.3,5 Acute clinical assessment and management of spinal cord-injured patients requires a skillful neurological examination and knowledge of multisystem management issues (cardiac, hemodynamic, pulmonary, urogenital) specific to this patient population, with the preeminent objective of medical and neurological stabilization and prevention of secondary injury. The primary focus of this chapter is to review the typical fractures or fracture dislocations that occur at a given vertebral column level and identify optimal nonsurgical or surgical treatment options. Generally, the decision for surgical intervention in spinal column injury is based on numerous factors, including, but certainly not limited to, degree of spinal deformity, biomechanical stability, and neurological status. Regardless of level, the principal management objectives are preservation of neurological function, prevention of secondary injury, and provision of an optimal milieu for neurological recovery.6–10 Frequently, the injured patient will require reduction of deformity, decompression of neural elements, and stabilization to achieve these goals. Early, and often urgent, surgical treatment is preferred if biomechanical stability of the spine is severely compromised or if neurological deficit is imminent or progressive. Yet, even the definitions of early and delayed remain controversial, and neurological outcomes are equivalent irrespective of timing of surgical intervention.6–8,10 Pulmonary failure and pneumonia are the leading causes of death in patients with spine trauma and SCI.1,9 Recent studies, however, emphasize the nonneurological benefits afforded by earlier surgical intervention when appropriate. Early surgical stabilization allows for more rapid mobilization and rehabilitation and has been shown to decrease complications such as pneumonia, decubitus ulcer formation, deep vein thrombosis, and urinary tract infections.9,10 Stability of the atlanto-occipital junction relies primarily on the integrity of the ligamentous structures: (1) anterior and posterior atlanto-occipital membranes, (2) tectorial membrane, (3) cruciate ligament, (4) apical ligament of the dens,and (5) alar ligaments. The tectorial membrane and alar ligaments are the principal structures in maintaining atlanto-occipital stability, and disruption of these structures results in an unstable injury. Figure 19-1 Midsagittal T2-weighted magnetic resonance imaging images show an atlanto-occipital dislocation. High signal intensity present in the ligamentous complex and spinal cord reflects severe injury to these structures. Traumatic atlanto-occipital dislocations (AODs) (Fig. 19-1) are uncommon injuries caused by hyperflexion and distraction forces during high-energy blunt trauma.3–5 Though often fatal, improvements in emergent patient management, transport, and early recognition have resulted in more survivors of AOD. Nearly 20% of survivors may show no initial focal neurological deficit, leading to a low suspicion for diagnosis of AOD.5,11 Consequently, 36% of patients with undiagnosed AOD experience neurological deterioration from inadequate cervical immobilization.5,11 In other cases where AOD is suspected, patients often have significant neurological deficits that include lower cranial nerve neuropathies, unilateral or bilateral weakness, or quadriplegia resulting from compression or distortion of the lower cranial nerves, brainstem, or spinal cord.3,5 Therefore, early identification and management of these injuries may limit progression of further neurological impairment.3,5,11,12 Although several radiographic methods based on the relationship between the skull base and cervical spine have been well described to diagnose AOD from lateral cervical spine radiographs (Table 19-1), the diagnosis from plain radiographic film is often missed.5 Because of this, additional imaging of the occipitocervical junction with reconstructive computed tomography (CT) or magnetic resonance imaging (MRI) should be considered. Moreover, the presence of prevertebral soft-tissue swelling or an increase in the dens-basion distance on lateral cervical spine radiograph, or subarachnoid hemorrhage at the craniovertebral junction on CT may provide diagnostic clues.3,5,11 Atlanto-occipital dislocation injuries have been classified into four types based on the ligamentous injury pattern, all of which are unstable (Table 19-2).3,5 Initial treatment is immobilization of the cervical spine, preferably with a halo orthosis. Rigid cervical collars and traction are not recommended because they may exacerbate or produce distraction, promoting further injury. Nonoperative management alone is inadequate and has been found to lead to persistent instability and worsening neurological function.3,12,13 Thus definitive treatment for stabilization of AOD injuries is occipitocervical arthrodesis and rigid internal fixation, often accompanied by decompression and reduction to maximize neurological recovery.3,5,12 Although not true fractures, isolated traumatic transverse atlantal ligament injuries are unstable, result from high-energy flexion forces to the cervical spine, and are often associated with significant upper cervical SCI.14 Diagnosis may be made from lateral flexion cervical radiographs demonstrating a widened atlantodental interval, CT imaging showing a C1 lateral mass avulsion fracture, or by direct visualization with MRI. Two categories of injury are disruption of the ligament alone (type I) or with avulsion of the tubercle connecting the ligament to the C1 lateral mass (type II) (Table 19-2). Although type II injuries may occasionally be successfully treated nonoperatively with rigid cervical immobilization, results are often unsatisfactory and C1-C2 fusion is the treatment of choice. Type I ligamentous injuries do not heal with external immobilization and require surgical stabilization. Surgical options include C1-C2 arthrodesis supplemented by posterior wiring, transarticular screws, and/or segmental screw fixation.3,15
Epidemiology
General Consideration Regarding Timing of Surgical Treatment
Occipitocervical Junction Injuries
Atlantoaxial Ligamentous Injuries
| Method | Anatomical Relationship |
| Wackenheim’s clival line | Tangential line along posterior clivus to odontoid tip with no posterior or anterior displacement |
| Power’s ratio (BC:OA) | Distance ratio between basion to C1 posterior arch (BC) and opisthion to anterior C1 arch ≤1 |
| Wholey dens-basion technique | Distance from basion to dens ≤10 mm |
| Dublin’s method | Distance from posterior mandible to anterior atlas ≤ 13 mm; or distance from posterior mandible to dens ≤ 20 mm |
| Harris BAI-BDI method* | Basion to posterior C2 line [basion-axial interval (BAI)] with the caudal cortical line of the axis ≤12 mm ventrally or ≤4 mm dorsally; and basion to dens [basion-dens interval (BDI)] distance ≤12 mm |
* Most reliable means to diagnose atlanto-occipital dislocation.
| Type | Description of Disruption |
| CERVICAL FRACTURES1,3 | |
| Atlanto-occipital dislocations | |
| I | Anterior ligament dislocation |
| II | Longitudinal ligament dislocation |
| III | Posterior ligament dislocation |
| Other | Complex dislocation |
| Atlantoaxial ligamentous injuries | |
| IA | Midportion of transverse ligament |
| IB | Periosteal insertion with no bony fracture |
| IIA | Disconnection with C1 lateral mass with comminuted fracture |
| IIB | Disconnection with C1 lateral mass with avulsion fracture |
| Isolated C1 fractures | |
| I | Posterior arch only, often bilateral |
| II | Unilateral fracture with lateral mass involvement |
| III | Burst-type fracture, involves three or more fractures through the anterior and posterior C1 ring; Jefferson fracture |
| Odontoid fractures | |
| I | Superior tip of the dens |
| II | Base of dens at junction between dens and C2 vertebral body |
| IIA | Type II with comminuted bone fracture at base of the dens with free bony fragments |
| III | Fracture extension into vertebral body |
| Hangman’s fractures | |
| I | Isolated hairline fracture of the neural arch posterior to the vertebral body; <3 mm subluxation of C2 on C3 |
| II | Disruption of the posterior longitudinal ligament and the disk space below C2; > 4 mm subluxation of C2 on C3 or> 11 degrees angulation |
| IIA | Type II with less displacement but greater angulation |
| III | Pars articularis fracture with bilateral facet dislocation at C2-C3 |
| C2 body fractures | |
| I | Vertical, coronal orientation |
| II | Vertical, sagittal orientation |
| III | Transverse, axial orientation |
| C1-C2 rotary subluxation | |
| I | Rotary displacement without anterior shift |
| II | Rotary displacement with anterior displacement 3-5 mm |
| III | Rotary displacement with anterior displacement > 5 mm |
| IV | Rotary displacement with posterior translation |
| Combined C1-C2 fractures | |
| See above for description of C2 fracture that typifies these injuries | |
| C1-type II odontoid | |
| C1-miscellaneous axis | |
| C1-type III odontoid | |
| C1-hangman’s-type | |
| SUBAXIAL C3-C7 CERVICAL COLUMN FRACTURES1,3 | |
| Distractive flexion | Flexion dislocation injuries with variable ligamentous damage involving the ligamentum flavum, interspinous ligaments, posterior longitudinal ligament, and dorsal facet capsule complex (posterior ligamentous complex) |
| Distractive extension | Failure of anterior ligamentous complex with widening of the disk space and posterior distraction with possible variable injury to posterior ligamentous complex |
| Compressive flexion | Vertebral body and posterior ligamentous complex disruption to varying degrees; “teardrop” fractures |
| Compressive extension | Varied involvement of vertebral arch and laminar fractures with displacement of vertebral body |
| Vertical compression | Cervical burst-type fracture usually associated with vertebral body fracture and displacement |
| THORACIC, THORACOLUMBAR AND LUMBAR FRACTURES1,3,28 | |
| Compression | Failure of the anterior column with varying degrees of loss of height |
| Burst | Failure of anterior and middle columns from pure axial loading on vertebral body |
| Seat-belt type | Failure of posterior and middle columns due to flexion forces |
| Fracture dislocations | Failure of anterior, middle, and posterior columns due to combined compression, rotation, tension, or shear forces resulting in varying degrees of subluxation or distraction |
Isolated C1 Fractures
Atlas fractures (Fig. 19-2) account for ~2% to 13% of acute cervical spine fractures and occur typically with axial load trauma, with or without lateral bending.3,5,14 Any part of the C1 ring or lateral mass may be involved and fractures typically occur at multiple sites (Table 19-2). A Jefferson fracture is classically referred to as a four-point fracture (bilateral anterior and posterior ring) but more recently includes the more common two- or three-point fractures.5 Neurological deficit is rare and likely due to the larger spinal canal at this level and the tendency of the bone fragments to burst outward.3 Assessment of C1 fractures for stability is dependent on the integrity of the transverse ligament, which may be evaluated by odontoid plain radiographs or direct visualization with high-resolution MRI. Generally, the transverse ligament is considered disrupted if the sum of displacement of the lateral masses of C1 over C2 is greater than 6.9 mm (rule of Spence) or the atlantodental interval is greater than 3 mm observed in the odontoid view radiograph.16
Both isolated stable or unstable C1 fractures have been effectively managed with rigid external immobilization for 8 to 12 weeks. Operative management may be considered for burst fractures with transverse atlantal ligamentous injury. Stabilization may be achieved by arthrodesis supplemented by posterior (or anterior) C1-C2 transarticular screws, C1 lateral mass-C2 pars/pedicle screws, or occipital-C1-C2 constructs. Wiring techniques are generally ineffective because they often fail to fixate the load-bearing lateral masses. The type of internal fixation performed may influence the requirement for postoperative immobilization.5,16










