Chapter 9 Depression and Psychosis in Neurological Practice
The most widely recognized nomenclature used for discussion of mental disorders derives from the classification system developed for the Diagnostic and Statistical Manual of Mental Disorders (DSM). The American Psychiatric Association introduced the DSM in 1952 to facilitate psychiatric diagnosis through improved standardization of nomenclature. There have been consecutive revisions of this highly useful and relied-upon document since its inception, with the last revision being the DSM IV-TR in 2000 and a planned revision, the DSM V, scheduled for publication in 2013. Discussion about the potential secondary causes of depression and psychosis requires a familiarity with the most salient features of the primary psychiatric conditions. A brief outline of selected conditions derived from the DSM IV-TR is included in Boxes 9.1 and 9.2, which can be found at www.expertconsult.com, along with other content in this chapter marked “online only.”
Box 9.1 Diagnostic Features of Primary Psychiatric Disorders
Schizophrenia is a disorder that lasts for at least 6 months and includes at least 1 month of active symptoms (two or more of the following: delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, or negative symptoms).
Schizoaffective disorder is a disorder in which a mood episode and the active symptoms of schizophrenia occur together and were preceded or are followed by at least 2 weeks of delusions or hallucinations without prominent mood symptoms.
Major depressive disorder is characterized by one or more major depressive episodes (at least 2 weeks of depressed mood or loss of interest accompanied by at least four additional symptoms of depression). Additional symptoms of depression may include significant weight loss or loss of appetite, sleep dysfunction, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness or guilt, cognitive problems, and suicidal ideational or thoughts of death.
A manic episode is defined by an abnormally and persistently elevated, expansive, or irritable mood persisting for at least 1 week (or less if hospitalization is required). At least three of the following symptoms must be present if the mood is elevated or expansive (four symptoms are required if the mood is irritable): inflated self esteem or grandiosity, decreased need for sleep, pressured speech, flight of ideas, distractibility, increased goal directed activities or psychomotor agitation, and excessive involvement in pleasurable activities with a high potential for painful consequences. Psychotic features may be present.
Bipolar I disorder is characterized by the presence of both manic and major depressive episodes or manic episodes alone.
Bipolar II is characterized by the presence of major depressive episodes alternating with episodes of hypomania.
Hypomania is characterized by an abnormally and persistently elevated, expansive, or irritable mood persisting for at least 4 days. Other criteria required for diagnosis are identical to that of a manic episode except that the symptoms are not so severe as to cause marked impairment in social or occupational functioning, hospitalization is not required, and no psychotic symptoms are present.
Box 9.2 Psychiatric Terms of Relevance to Neurologists
Abulia is the state of reduced impulse to act and think associated with indifference about consequences of action.
Affect is the examiner’s observation of the patient’s emotional state. Frequently used descriptive terms include:
Anxiety is the feeling of apprehension caused by anticipation of danger that may be internal or external.
Apathy is dulled emotional tone associated with detachment or indifference.
Comportment refers to self-regulation of behavior through complex mental processes that include insight, judgment, self-awareness, empathy, and social adaptation.
Compulsion is the uncontrollable impulse to perform an act repetitively.
Confusion is the inability to maintain a coherent stream of thought owing to impaired attention and vigilance. Secondary deficits in language, memory, and visual spatial skills are common.
Delusion is a false, unshakable conviction or judgment that is out of keeping with reality and with socially shared beliefs of the individual’s background and culture. It cannot be corrected with reasoning.
Depression is a sustained psychopathological feeling of sadness often accompanied by a variety of associated symptoms, particularly anxiety, agitation, feelings of worthlessness, suicidal ideation, abulia, psychomotor retardation, and various somatic symptoms and physiological dysfunctions and complaints that cause significant distress and impairment in social functioning.
Hallucination is a false sensory perception not associated with real external stimuli.
Mood is the emotional state experienced and described by the patient and observed by others.
Obsession is the pathological persistence of an irresistible thought or feeling that cannot be eliminated from consciousness by logical effort. It is associated with anxiety and rumination.
Paranoia is a descriptive term designating either morbid dominant ideas or delusions of self-reference concerning one or more of several themes, most commonly persecution, love, hate, envy, jealousy, honor, litigation, grandeur, or the supernatural.
Prosody is the melodic patterns of intonation in language that convey shades of meaning.
Psychosis is the inability or impaired ability to distinguish reality from hallucinations and/or delusions.
Thought process and content. Common descriptive terms include:
Principles of Differential Diagnosis
Emotional and cognitive processes are based on brain structure and physiology. Abnormal behavior can be attributable to the complex interplay of social influences, physical environment, and neural physiology. Psychosis, mania, depression, disinhibition, obsessive compulsive disorder (OCD), and anxiety all can occur as a result of neurological disease and can be indistinguishable from the idiopathic forms (Robinson and Travella, 1996). Neurological conditions must be considered in the differential diagnosis of any disorder with psychiatric symptoms.
Neuropsychiatric dysfunction can be correlated with altered functioning in anatomical regions. Any disease, toxin, drug, or process that affects a particular region can be expected to show changes in behavior mediated by the circuits within that region. The limbic system and the frontosubcortical circuits are most commonly involved in neuropsychiatric dysfunction. This neuroanatomical conceptual framework can provide useful information for localization and thus differential diagnosis. Klüver-Bucy syndrome, which consists of placidity, apathy, visual and auditory agnosia, hyperorality, and hypersexuality, occurs in processes that cause injury to the bilateral medial temporoamygdalar regions. A few of the most common causes of this syndrome include herpes encephalitis, traumatic brain injury (TBI), frontotemporal dementias (FTDs), and late-onset or severe Alzheimer disease (AD). Brain trauma, ischemic disease, demyelination, abscesses, or tumors, as well as degenerative dementias can also result in disinhibition. Damage to any portion of the circuit between the orbitofrontal cortex, ventral caudate nucleus, anterior globus pallidus, or mediodorsal thalamus can result in disinhibition (Tekin and Cummings, 2002).
Mood disorders, paranoia, disinhibition, and apathy derive from dysfunction in the limbic system and basal ganglia, which are phylogenetically more primitive (Mesulam, 2000). In some cases, the behavioral changes represent a response to the underlying disability; in others, behavioral abnormalities are part of the disease. For example, studies have shown that apathy in Parkinson disease (PD) is probably related to the underlying disease process, rather than being a psychological reaction to disability or to depression, and is closely associated with cognitive impairment (Kirsch-Darrow et al., 2006). Positron emission tomographic (PET) and single-photon emission computed tomographic (SPECT) studies suggest similar regions of abnormality in acquired forms of depression, mania, OCD, and psychosis, compared with their primary psychiatric presentations (Hirono et al., 1998; Rubinsztein et al., 2001; Saxena et al., 1998). Table 9.1 summarizes neuropsychiatric symptoms and their anatomical correlates. Additionally, the developmental phase during which a neurological illness occurs influences the frequency with which some neuropsychiatric syndromes are manifested. Adults with post-TBI sequelae tend to exhibit a higher rate of depression and anxiety. In contrast, post-TBI sequelae in children often involve attention deficits, hyperactivity, irritability, aggressiveness, and oppositional behavior (Geraldina et al., 2003). When temporal lobe epilepsy or Huntington disease (HD) begins in adolescence, a higher incidence of psychosis is noted than when their onset occurs later in life. Earlier onset of multiple sclerosis (MS) and stroke are associated with a higher incidence of depression (Rickards, 2005).
Table 9.1 Neuropsychiatric Symptoms and Corresponding Neuroanatomy
| Symptom | Neuroanatomical Region |
|---|---|
| Depression | Frontal lobes, left anterior frontal cortex, anterior cingulate gyrus, subgenu of the corpus callosum, basal ganglia, left caudate |
| Mania | Inferomedial and ventromedial frontal cortex, right inferomedial frontal cortex, anterior cingulate, caudate nucleus, thalamus, and temporothalamic projections |
| Apathy | Anterior cingulate gyrus, nucleus accumbens, globus pallidus, thalamus |
| OCD | Orbital or medial frontal cortex, caudate nucleus, globus pallidus |
| Disinhibition | Orbitofrontal cortex, hypothalamus, septum |
| Paraphilia | Mediotemporal cortex, hypothalamus, septum, rostral brainstem |
| Hallucinations | Unimodal association cortex, orbitofrontal cortex, paralimbic cortex, limbic cortex, striatum, thalamus, midbrain |
| Delusions | Orbitofrontal cortex, amygdala, striatum, thalamus |
| Psychosis | Frontal lobes, left temporal cortex |
OCD, Obsessive-compulsive disorder.
Patients with AD, PD, HD, and FTDs can develop multiple coexisting symptoms such as irritability, agitation, impulse-control disorders, apathy, depression, delusions, and psychosis that may be exacerbated by medications used to treat the underlying disorder (Table 9.2). For example, in patients with PD dopamine agonists such as pramipexole and ropinirole have been found to increase the risk of pathological gambling, compulsive shopping, hypersexuality, and other impulse-control disorders, sometimes referred to as dopamine dysregulation (Voon et al., 2006; Weintraub et al., 2006). Management outcome can be influenced by multiple factors. For instance, the complex relationship between behavioral changes and the caregiver’s ability to cope play a role in illness management and nursing home placement (de Vugt et al., 2005; Smith et al., 2001). Behavioral disturbances in patients with neurological illness have been related to the severity of caregiver distress (Kaufer et al., 1998).
Table 9.2 Neurological Disorders and Associated Prominent Behavioral Features
| Neurological Disorder | Associated Behavioral Disturbances |
|---|---|
| Alzheimer disease | Depression, irritability, anxiety, apathy, delusions, paranoia, psychosis |
| Lewy body dementia | Fluctuating confusion, hallucinations, delusions, depression, RBD |
| Vascular dementia | Depression, apathy, psychosis |
| Parkinson disease | Depression, anxiety drug-associated hallucinations and psychosis, RBD |
| FTD | Early impaired judgment, disinhibition, apathy, depression, delusions, psychosis |
| PSP | Disinhibition, apathy |
| TBI | Depression, disinhibition, apathy, irritability, psychosis uncommon |
| HD | Depression, irritability, delusions, mania, apathy, obsessive-compulsive disorder, psychosis |
| Corticobasal degeneration | Depression, irritability, RBD, alien hand syndrome |
| Epilepsy | Depression, psychosis |
| HIV infection | Apathy, depression, mania, psychosis |
| MS | Depression, irritability, anxiety, euphoria, psychosis |
| ALS | Depression, disinhibition, apathy, impaired judgment |
ALS, Amyotrophic lateral selerosis; FTD, frontotemporal dementia; HD, Huntington disease; HIV, human immunodeficiency virus; MS, multiple sclerosis; OCD, obsessive-compulsive disorder; PSP, progressive supranuclear palsy; RBD, rapid eye movement behavior disorder; TBI, traumatic brain injury.
Principles of Neuropsychiatric Evaluation
1. A normal neurological examination does not exclude neurological conditions. Lesions in the limbic, paralimbic, and prefrontal regions may manifest with cognitive-behavioral changes in the absence of elemental neurological abnormalities.
2. Normal routine laboratory testing, brain imaging, electroencephalography, and cerebral spinal fluid analysis do not necessarily exclude diseases of neurological origin.
3. New neurological complaints or behavioral changes should not be dismissed as being of psychiatric origin in a person with a preexisting psychiatric history.
4. The possibility of iatrogenically induced conditions such as lethargy with benzodiazepines, parkinsonism with neuroleptics, or hallucinations with dopaminergic medications must be taken into account. Medication side effects can significantly complicate the clinical history and physical examination in both the acute and long-term setting. Medication side effects can also potentially be harbingers of underlying pathology or progression of illness. Marked parkinsonism occurring after neuroleptic exposure can be a feature of PD and dementia with Lewy bodies (Aarsland et al., 2005) before the underlying neurodegenerative condition becomes clinically apparent. PD patients may develop hallucinations as a side effect of dopaminergic medications (Papapetropoulos and Mash, 2005).
5. Treatment of primary psychiatric and neurological behavioral disturbances share common principles. A response to therapy does not constitute evidence for a primary psychiatric condition.
The medical evaluation of affective illness and psychotic disorders must be individualized based on the patient’s family history, social environment, habits, risk factors, age, gender, clinical history, and examination findings. A careful review of the patient’s medical history and a general physical examination as well as a neurological examination (Murray and Price, 2008; Ovsiew et al., 2008) should be performed to assess for possible neurological and medical causes. The most basic evaluation should include vital signs (blood pressure, pulse, respirations, and temperature) and a laboratory evaluation that minimally includes a complete blood cell count (CBC); electrolyte panel; determination of serum levels for glucose, blood urea nitrogen (BUN), creatinine, calcium, total protein, and albumin; liver function assessment; thyroid function assessment; and additional laboratory testing as clinically indicated. Consideration should be given to checking the patient’s oxygen saturation on room air (especially in the elderly). Neurological abnormalities suggested by the clinical history or identified on examination, especially those attributable to the central nervous system (CNS), should prompt further evaluation for neurological and medical causes of psychiatric illness. A clear consensus has not been reached about when neuroimaging is indicated as part of the evaluation of new-onset depression in patients without focal neurological complaints and a normal neurological examination. This must be individualized based on clinical judgment. Treatment-resistant depression should prompt reassessment of the diagnosis and evaluation to rule out secondary causes of depressive illness. A careful history to rule out a primary sleep disorder such as sleep apnea should be considered in the evaluation of refractory depressive symptoms (Haba-Rubio, 2005) or cognitive complaints. When new-onset psychosis presents in the absence of identifiable infectious/inflammatory, metabolic, toxic, or other causes, we recommend that magnetic resonance imaging (MRI) of the brain be incorporated into the evaluation. In our experience, 5% to 10% of such patients have MRI abnormalities that identify potential neurological contributions (particularly in those 65 years of age and older). The MRI will help exclude lesions (e.g., demyelination, ischemic disease, neoplasm, congenital structural abnormalities, evidence of metabolic storage diseases) in limbic, paralimbic, and frontal regions, which may not be associated with neurological abnormalities on elemental examination (Walterfang et al., 2005). An electroencephalogram (EEG) should be considered to evaluate for complex partial seizures if there is a history of intermittent, discrete, or abrupt episodes of psychiatric dysfunction (e.g., confusion, spells of lost time, psychotic symptoms), stereotypy of hallucinations, automatisms (e.g., lip smacking, repetitive movements) associated with episodes of psychiatric dysfunction (or confusion), or a suspicion of encephalopathy (or delirium). Sensitivity of the EEG for detecting seizure activity is highest when the patient has experienced the specific symptoms while undergoing the study. Selected cases may require 24-hour or longer EEG monitoring to capture a clinical event to clarify whether a seizure disorder is present.
Cognitive-Behavioral Neuroanatomy
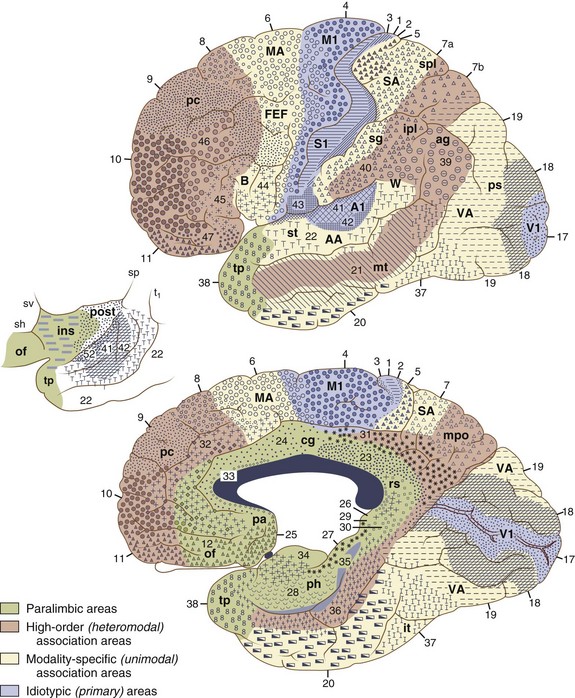
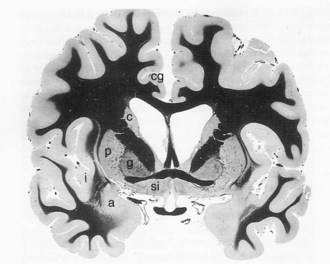
The cerebral cortex can be subdivided into five major functional subtypes: primary sensory-motor, unimodal association, heteromodal association, paralimbic, and limbic. The primary sensory areas are the point of entry for sensory information into the cortical circuitry. The primary motor cortex conveys complex motor programs to motor neurons in the brainstem and spinal cord. Processing of sensory information occurs as information moves from primary sensory areas to adjacent unimodal association areas. The unimodal and heteromodal cortices are involved in perceptual processing and motor planning. The complexity of processing increases as information is then transmitted to heteromodal association areas which receive input from more than one sensory modality. Examples of heteromodal association cortex include prefrontal cortex, posterior parietal cortex, parts of the lateral temporal cortex, and portions of the parahippocampal gyrus. These cortical regions have a six-layered architecture. Further cortical processing occurs in areas designated as paralimbic. These regions demonstrate a gradual transition of cortical architecture from the six-layered to the more primitive and simplified allocortex of limbic structures. The paralimbic regions consist of orbitofrontal cortex, insula, temporal pole, parahippocampal cortex, and cingulate cortex. Cognitive, emotional, and visceral inputs merge in these regions. The limbic subdivision is composed of the hippocampus, amygdala, substantia innominata, prepiriform olfactory cortex, and septal area (Figs. 9.1 and 9.2). These structures are to a great extent reciprocally interconnected with the hypothalamus. The limbic region is intimately involved with regulation of emotion, memory, motivation, autonomic, and endocrine function. The highest level of cognitive processing occurs in regions referred to as transmodal areas. These areas are composed of heteromodal, paralimbic, and limbic regions, which are collectively linked, in parallel, to other transmodal regions. Interconnections among transmodal areas (e.g., Wernicke area, posterior parietal cortex, hippocampal-enterorhinal complex) allow integration of distributed perceptual processing systems, resulting in perceptual recognition such as scenes and events becoming experiences and words taking on meaning (Mesulam, 2000).
Cortical Networks
Five distinct cortical network regions govern various aspects of cognitive functioning: (1) the language network, which includes transmodal regions or “epicenters” in Broca and Wernicke areas; (2) spatial awareness, based in transmodal regions in the frontal eye fields and posterior parietal area; (3) the memory and emotional network, located in the hippocampal-enterorhinal region and amygdala; (4) the executive function–working memory network, based in transmodal regions in the lateral prefrontal cortex and possibly the inferior parietal cortices; and (5) the face-object recognition network, based in the temporopolar and midtemporal cortices (Mesulam, 1998).
The ability to empathize with another person’s psychological and physical circumstances is a foundation for social and moral behavior. The human mirror neuron system is now postulated to be involved in understanding the actions of others and the intentions behind the actions. It also may provide the basis for observational learning. The parietofrontal mirror system, which includes the parietal lobe and the premotor cortex plus the caudal part of the inferior frontal gyrus, is involved in recognition of voluntary behavior in other people, while the limbic mirror system, formed by the insula and the anterior mesial frontal cortex, is devoted to the recognition of affective behavior. Dysfunction of this system is postulated to underlie deficits in theory of mind and has been proposed as an explanation for the social deficits seen in autistic disorders (Cattaneo and Rizzolatti, 2009).
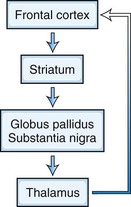
Frontosubcortical Networks
Five frontosubcortical circuits subserve cognition, behavior, and movement. Disruption of these networks at the cortical or subcortical level can be associated with similar neuropsychiatric symptoms. Each of these circuits shares the same components: (1) frontal cortex, (2) striatum (caudate, putamen, ventral striatum), (3) globus pallidus and substantia nigra, and (4) thalamus (which then projects back to frontal cortex) (Tekin and Cummings, 2002) (Fig. 9.3). Integrative connections also occur to and from other subcortical and distant cortical regions related to each circuit. Neurotransmitters such as dopamine (DA), glutamate, γ-aminobutyric acid (GABA), acetylcholine, norepinephrine, and serotonin are involved in various aspects of neural transmission and modulation in these circuits. The frontosubcortical networks are named according to their site of origin or function. Somatic motor function is subserved by the motor circuit originating in the supplementary motor area. Oculomotor function is governed by the oculomotor circuit originating in the frontal eye fields. Three of the five circuits are intimately involved in cognitive and behavioral changes: the dorsolateral prefrontal, the orbitofrontal, and the anterior cingulate circuits. Each circuit has both efferent and afferent connections with adjacent and distant cortical regions. The dorsolateral prefrontal circuit governs executive functions, including the ability to plan and maintain attention, problem solve, learn, retrieve remote memories, sequence the temporal order of events, shift cognitive and behavioral sets, and generate motor programs. Executive dysfunction is a principal component of subcortical dementias. Deficits identified in subcortical dementias include slowed information processing, memory retrieval deficits, mood and behavioral changes, gait disturbance, dysarthria, and other motor impairments. Vascular dementias, PD, and HD are a few examples of conditions that affect this circuit.
The orbitofrontal circuit connects frontal monitoring functions to the limbic system. This circuit governs appropriate responses to social cues, empathy, social judgment, and interpersonal sensitivity. It pairs thoughts, memories, and experiences with corresponding visceral and emotional states. This circuit is heavily involved in the process of decision making and evaluating the costs and benefits of specific behavioral responses to the environment. The medial orbitofrontal cortex (OFC) evaluates reward, whereas the lateral OFC monitors and decodes punishment as it pertains to motivating behavioral change. There is also an anterior-posterior gradient in which the reward value for more abstract and complex secondary reinforcing factors such as money are encoded in the anterior regions, and more concrete factors such as touch and taste are encoded in the posterior OFC areas. The posterior OFC is thought to have an important role in evaluating the emotional significance of stimuli (Barbas and Zikopoulos, 2007). Dysfunction in this circuit can lead to disinhibition, irritability, aggressive outbursts, inappropriate social responses, and impulsive decision making. Patients with OFC lesions show deficits in both the production and recognition of emotional expression from the face, voice, or gestures. Persons with bilateral OFC lesions may manifest “theory of mind” deficits. Theory of mind is a model of how a person understands and infers other people’s intentions, desires, mental states, and emotions (Bodden et al., 2010). Conditions that exhibit impairment in this circuit include schizophrenia (Bora et al., 2009), FTD (Adenzato et al., 2010), and HD. Other conditions that may affect this circuit include closed head trauma, rupture of anterior communicating aneurysms, and subfrontal meningiomas.
The anterior cingulate circuit includes the nucleus accumbens and has both afferent and efferent connections to the dorsolateral prefrontal cortex (DLPFC) and amygdala. It is involved in motivated behavior. Lesions in this circuit result in apathy, abulia, and akinetic mutism. There also is a reported decrease in the ability to understand new thoughts and participate in the creative thought process (Chow and Cummings, 1999; Mesulam, 2000). The medial prefrontal cortex is thought to play a significant role in generating emotions related to empathy, cognitive functions related to theory of mind, and the ability to recognize a moral dilemma (Robertson et al., 2007). The ventromedial frontal lobe evaluates the current relative value of stimuli helping to guide decision making by determining the goals toward which behavior is directed and through judging outcomes (Fellows, 2007). Some conditions that may affect this circuit include AD, FTD, PD, HD, head trauma, brain tumors, cerebral infarcts, and obstructive hydrocephalus.
Cerebrocerebellar Networks
The cerebellum is engaged in the regulation of cognition and emotion through a feed-forward and feedback loop. The cortex projects to pontine nuclei, which in turn project to the cerebellum. The cerebellum projects to the thalamus, which then projects back to the cortex. Cognitive processing tasks such as language, working memory, and spatial and executive tasks appear to activate the posterior cerebellar lobe. The posterior cerebellar vermis may function as a putative limbic cerebellum, modulating emotional processing (Stoodley and Schmahmann, 2010). Distractibility, executive and working memory problems, impaired judgment, reduced verbal fluency, disinhibition, irritability, anxiety, emotional lability or blunting, obsessive compulsive behaviors, depression, and psychosis have been reported in association with cerebellar pathology.
Biology of Psychosis
Among several etiological hypotheses for schizophrenia, the neurodevelopmental model is one of the most prominent. This model generally posits that schizophrenia results from processes that begin long before the onset of clinical symptoms and is caused by a combination of environmental and genetic factors (Murray and Lewis, 1987; Weinberger, 1987). Several postmortem and neuroimaging studies support this hypothesis with findings of brain developmental alterations such as agenesis of the corpus callosum, arachnoid cysts, and other abnormalities in a significant number of schizophrenic patients (Hallak et al., 2007; Kuloglu et al., 2008). Environmental factors are associated with an increased risk for schizophrenia. These factors include being a first-generation immigrant or the child of a first-generation immigrant, urban living, drug use, head injury, prenatal infection, maternal malnutrition, obstetrical complications during delivery, and winter birth (Tandon et al., 2008). Genetic risks are clearly present but not well understood. The majority of patients with schizophrenia lack a family history of the disorder. The population lifetime risk for schizophrenia is 1%, 10% for first-degree relatives, and 4% for second-degree relatives. There is an approximately 50% concordance rate for monozygotic twins, compared to approximately 15% for dizygotic twins. Advancing paternal age increases risk in a linear fashion, which is consistent with the hypothesis that de novo mutations contribute to the genetic risk for schizophrenia. It is most likely that many different genes make small but important contributions to susceptibility. The disease only manifests when these genes are combined or certain environmental factors are present. A number of susceptibility genes show association with schizophrenia: catechol-O-methyl-transferase, neuroregulin 1, dysbindin, disrupted in schizophrenia 1 (DISC1), metabotropic glutamate receptor type 3 gene and G27/G30 gene complex (Nöthen et al., 2010; Tandon et al., 2008). Research in twins and first-degree relatives of patients has shown that genes predisposing to schizophrenia and related disorders affect heritable traits related to the illness. Such traits include neurocognitive functioning, structural MRI brain volume measures, neurophysiological informational processing traits, and sensitivity to stress (van Os and Kapur, 2009). A small proportion of schizophrenia incidence may be explained by genomic structural variations known as copy number variants (CNVs). CNVs consist of inherited or de novo small duplications, deletions, or inversions in genes or regulatory regions. CNV deletions generally show higher penetrance (more severe phenotype) than duplications, and larger CNVs often have higher penetrance and/or more clinical features than smaller CNVs. These genomic structural variations contribute to normal variability, disease risk, and developmental anomalies, as well as act as a major mutational mechanism in evolution. The most common CNV disorder, 22q11.2 deletion syndrome (velocardiofacial syndrome), has an established association with schizophrenia. Individuals with 22q11.2 deletions have a 20-fold increased risk for schizophrenia and constitute about 0.9% to 1% of schizophrenia patients. When this syndrome is present, genetic counseling is helpful (Bassett and Chow, 2008).
A wide variety of neurological conditions, medications, and toxins are associated with psychosis. No consensus is available in the literature regarding the precise anatomical localization of various psychotic syndromes. Evidence from neurochemistry, cellular neuropathology, and neuroimaging studies support that schizophrenia is a brain disease, but there is no universally accepted theory regarding the specific nature of the brain dysfunction. The two best-known neurotransmitter models offered to explain the various manifestations of schizophrenia include the “dopamine hypothesis,” now in its third revision (Howes and Kapur, 2009), and the “glutamate hypothesis.” Schizophrenia has been associated with frontal lobe dysfunction and abnormal regulation of subcortical DA (Goldman-Rakic et al., 2004) and glutamate systems (Weinberger, 2005).
Functional imaging studies in persons with schizophrenia show decreased cerebral blood flow (CBF) in the DLPFC during specific cognitive tasks (Andreasen, 1996; Lehrer et al., 2005). Schizophrenic patients with prominent negative symptoms display reduced glucose utilization in the frontal lobes. Functional imaging studies suggest that disruption in distributed functional circuits is important in the development of schizophrenia. These functional circuit locations include the DLPFC, orbitofrontal cortex, mediofrontal cortex, anterior cingulate gyrus, thalamus, temporal lobe subregions, and the cerebellum (Schultz and Andreasen, 1999). Several conditions that may manifest psychosis (e.g., HD, PD, frontotemporal degenerations, stroke) are commonly associated with frontal and subcortical dysfunction. Dorsolateral and mediofrontal hypoperfusion on functional imaging has been demonstrated in a subset of AD patients with delusions (Hirono et al., 1998).
Biology of Depression
The connection between psychiatry and neurology is nowhere more evident than the remarkable comorbidity of psychiatric illness, especially depression, in many neurological disorders, with a 20% to 60% prevalence rate of depression in patients with stroke, neurodegenerative diseases, MS, headache, human immunodeficiency virus (HIV), TBI, epilepsy, chronic pain, obstructive sleep apnea, intracranial neoplasms, and motor neuron disease. Depression amplifies the physiological response to pain, while pain-related symptoms and limitations frequently lead to the emergence of depressive symptoms. In a community-based study, almost 50% of adolescents with chronic daily headaches had at least one psychiatric disorder, most commonly major depression and panic. Women with migraine who have major depression are twice as likely as those with migraine alone to report being sexually abused as a child. If the abuse continued past age 12, women with migraine were five times more likely to report depression (Tietjen et al., 2007). Despite the proliferation of antidepressant therapeutics, major depression is often a chronic and/or recurrent condition that remains difficult to treat. Up to 70% of patients taking antidepressants in a primary care setting may be poorly compliant, most often due to adverse side effects during both short and long-term therapy.
Efforts to link single genes to major depressive disorder (MDD) have been unsuccessful despite exhaustive mapping attempts. Consequently, behavioral geneticists have turned to the study of genetic polymorphisms in establishing a predisposition to depression and in shaping the response to environmental stressors. Perlis and coworkers (2007) found a strong association between variation at the CREB1 locus and anger expression in MDD. The most extensive studies in this field have focused on polymorphisms in the serotonin transporter (5-HTT) gene. Recent work has demonstrated that patients with a single nucleotide polymorphism on the long allele that entails an A-to-G transposition (LG) have low expression of 5-HT. The risk for major depression among hurricane survivors with either short or LG alleles was four to five times that of low-risk survivors. Although conflicting results have been reported with regard to these polymorphisms, a recent meta-analysis found that the 44bp Ins/Del short/long polymorphism was associated with MDD, whereas the VNTR intron 2 polymorphism was not. This study also reported significant associations for polymorphisms in the apolipoprotein E, guanine nucleotide binding protein, methylenetetrahydrofolate reductase, and dopamine transporter genes (López-León et al., 2008).
Behavioral genetics research based on diathesis-stress models of depression demonstrate that the risk of depression after a stressful event is enhanced in populations carrying genetic risk factors and is diminished in populations lacking such risk factors. A gene’s contribution to depression may be missed in studies that do not account for environmental interactions and may only be revealed when studied within the context of environmental stressors specifically mediated by that gene (Uher, 2008). Genotype-environment interactions are ubiquitous because genes not only impact the risk for depression by creating susceptibility to specific environmental stressors but also cause individuals to persistently place themselves in highly stressful environments.
The potential clinical relevance of neurogenesis in the adult mammalian brain represents the most recent major breakthrough in depression studies at the cellular neurobiological level. Imaging studies have demonstrated a 10% to 20% decrease in the hippocampal volume of human patients with chronic depression. Cell proliferation studies using 5-bromo-2′-deoxyuridine injection to label dividing cells show that antidepressants also lead to increased cell number in the mammalian hippocampus. This effect is seen with chronic but not acute treatment; the time course of the effect mirrors the known time course of the therapeutic action of antidepressants in humans (Czéh et al., 2001). Although a role for neurogenesis in the pathophysiology of depression appears to be a promising avenue of research, the relevance of animal studies described here remains controversial in the human (Reif et al., 2006).
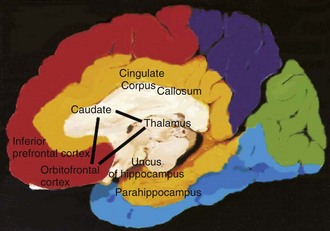
Analysis at the systems level suggests that anterotemporal paralimbic and orbitofrontal regions are involved in mediating primary and acquired depression. Functional imaging studies of unmedicated patients with familial depression reveal increased CBF and glucose metabolism in the amygdala, orbital cortex, and medial thalamus and decreased CBF and glucose metabolism in the dorsomedial/dorsal anterolateral prefrontal cortex and anterior cingulate cortex (Charney and Manji, 2004). Damage to the prefrontal cortex from stroke or tumor, or to the striatum from degenerative diseases such as PD and HD, is associated with depression (Charney and Manji, 2004; Drevets, 2001). Functional imaging studies of subcortical disorders such as these reveal hypometabolism in paralimbic regions, including the anterotemporal cortex and anterior cingulate, which are correlated with depression seen in these patients (Ketter et al., 1996; Mayberg, 2003). Depression in PD, HD, and epilepsy has been correlated with reduced metabolic activity in the orbitofrontal cortex and caudatenucleus.
Mayberg (2003) proposed that primary depression is due to dysfunction in a network that includes two known pathways: the orbitofrontal–basal ganglia–thalamic circuit and the basotemporal limbic circuit that links the orbitofrontal cortex and the anterior temporal cortex by the uncinate fasciculus. Portions of this model are illustrated in Fig. 9.4. This has been expanded into a unifying depression circuit model that consists of four interconnected functional compartments. Each functional compartment consists of strongly interconnected anatomical structures upon which that compartment is dependent. Functional compartments are as follows: mood regulation (medial frontal, medial orbital-frontal and pregenu anterior cingulate cortex), mood monitoring (ventral striatum-caudate, amygdale, dorsomedial thalamus, midbrain-ventral tegmental area), interoception (subcallosal cingulated, ventral-anterior hippocampus, anterior insula, brain stem, hypothalamus) and exteroception (prefrontal, premotor, parietal, mid-cingulate and posterior cingulate cortices with dorsal-posterior hippocampus) (Mayberg, 2009).
Functional imaging studies of untreated depression have been extended to evaluate responses to pharmacological, cognitive-behavioral, and surgical treatments of depression. Clinical improvement after treatment with serotonin-specific reuptake inhibitors such as fluoxetine correlates with increased activity on PET in brainstem and dorsal cortical regions including the prefrontal, parietal, anterior, and posterior cingulate areas, and with decreased activity in limbic and striatal regions including the subgenual cingulate, hippocampus, insula, and pallidum (Mathew et al., 2003). These findings are consistent with the prevailing model for involvement of a limbic-cortical-striatal-pallidal-thalamic circuit in major depression. The same group has shown that imaging can be used to identify patterns of metabolic activity predictive of treatment response. Hypometabolism of the rostral anterior cingulate characterized patients who failed to respond to antidepressants, whereas hypermetabolism characterized responders. Dougherty and coworkers (2003) used PET to search for neuroimaging profiles that might predict clinical response to anterior cingulotomy in patients with treatment-refractory depression. Responders displayed elevated preoperative metabolism in the left prefrontal cortex and the left thalamus. A combination of functional imaging and pharmacogenomic technologies might allow subsets of treatment responders to be classified and predicted more precisely than with either technology alone. Goldapple and coinvestigators (2004) used PET to study the clinical response of cognitive-behavioral therapy in patients with unipolar depression and found increases in hippocampus and dorsal cingulate and decreases in dorsal, ventral, and medial frontal cortex. The authors speculate that the same limbic-cortical-striatal-pallidal-thalamic circuit is involved but that differences in the direction of metabolic changes may reflect different underlying mechanisms of action of cognitive-behavioral therapy (CBT) and selective serotonin reuptake inhibitors (SSRIs).
Clinical Symptoms and Signs Suggesting Neurological Disease
Many neurological conditions have associated psychiatric symptoms. Psychiatrists and neurologists need to be intimately acquainted with features of the clinical history and examination that indicate the need for further investigation. Box 9.3 outlines some key features that have historically suggested an underlying neurological condition. Box 9.4 (online only at www.expertconsult.com) reviews some key areas of the review of systems that can be helpful when assessing for neurological and medical causes of psychiatric symptoms. Table 9.3 (online only at www.expertconsult.com) reviews abnormalities in the elemental neurological examination associated with diseases that can exhibit significant neuropsychiatric features.
Box 9.3 Historical Features Suggesting Neurological Disease in Patients with Psychiatric Symptoms
Box 9.4 Review of Systems with Possible Neuropsychiatric Relevance and Related Neurological Conditions
ALS, Amyotrophic lateral sclerosis; CNS, central nervous system; MS, multiple sclerosis.
Table 9.3 Neurological Abnormalities Suggesting Diseases Associated with Psychiatric Symptoms
| Examination Abnormalities | Disease(s) or Underlying Etiology |
|---|---|
| Vital signs: | |
| Marked hypertension | Hypertensive encephalopathy, serotonin syndrome, neuroleptic malignant syndrome, preeclampsia |
| Tachypnea | Delirium due to systemic infection |
| Hypoventilation | Hypoxia, alcohol withdrawal, sedative intoxication |
| Behavior: | |
| Alien hand syndrome | Corticobasal ganglionic degeneration |
| Cranial nerves: | |
| Visual field deficit | Stroke, mass, MS, lupus |
| Pupils: | |
| Argyll Robertson | Neurosyphilis |
| Unilateral dilation | Brain herniation, porphyria |
| Horner syndrome | Stroke, carotid disease, demyelinating disease |
| Ophthalmoplegia: | |
| Vertical gaze palsy | PSP |
| Mixed | Wernicke-Korsakoff syndrome, chronic basilar meningitis |
| Cornea: Kayser-Fleischer rings | Wilson disease |
| Lens: cataracts | Chronic steroids, Down syndrome |
| Fundi: | |
| Papilledema | Intracranial mass lesion, MS |
| Optic pallor | MS, porphyria, Tay-Sachs |
| Extrapyramidal | Parkinson disease, DLB, HD, stroke, WD, numerous others |
| Cerebellar | Alcohol, hereditary degenerative ataxias, paraneoplastic, medication toxicity |
| Motor neuron | ALS, FTD with motor neuron disease |
| Peripheral nerve | Adrenomyeloneuropathy, metachromatic leukodystrophy, B12 deficiency, porphyria |
| Gait: | |
| Apraxia | Normal pressure hydrocephalus, frontal network dementias |
| Spasticity | Stroke, MS |
| Bradykinesia | Multiinfarct dementia, PD, PSP, DLB |
ALS, Amyotrophic lateral sclerosis; DLB, dementia with lewy bodies; HD, Huntington disease; MS, multiple sclerosis; PSP, progressive supranuclear palsy; WD, Wilson disease.
Psychiatric Manifestations of Neurological Disease
Virtually any process that affects the neuroanatomical circuits described earlier can result in behavioral changes and psychiatric symptoms at some point. Psychiatric symptoms may be striking and precede any neurological manifestation by years. Table 9.4 (online only at www.expertconsult.com) lists conditions that can be associated with psychosis or depression. Box 9.5 summarizes some key points from the preceding discussion. A general overview and discussion of a number of major categories of neurological and systemic conditions with prominent neuropsychiatric features follows. More detailed information regarding the evaluation, natural history, pathology, and specific treatment recommendations for these conditions is beyond the scope of this chapter.
Box 9.5 Key Points
1. Affective and psychotic disorders may occur as a result of neurological disease and be indistinguishable from the idiopathic forms.
2. Neuropsychiatric and cognitive dysfunction can be correlated with altered functioning in anatomical regions.
3. Cortical processing of sensory information proceeds from its point of entry through association areas with progressively more complex interconnections with other regions having sensory, memory, cognitive, emotional, and autonomic information, resulting ultimately in perceptual recognition and emotional meaning for experiences.
4. Frontosubcortical circuits are heavily involved in cognitive and behavioral functioning. Disruption of frontal circuits at the cortical or subcortical level by various processes can be associated with similar neuropsychiatric symptoms.
5. Features of the patient’s clinical history and examination can be suggestive of a medical or neurological cause of psychiatric symptoms.
6. Many medical and neurological conditions are associated with neuropsychiatric symptoms. Each condition may carry unique implications for prognosis, treatment, and long-term management.
Table 9.4 Selected Neurological and Systemic Causes of Depression and/or Psychosis
| Category | Disorders |
|---|---|
| Head trauma | Traumatic brain injury |
| Subdural hematoma | |
| Infectious | Lyme disease |
| Prion diseases | |
| Neurosyphilis | |
| Viral infections/encephalitides (HIV infection/encephalopathy, herpes encephalitis, cytomegalovirus, Epstein-Barr virus, etc.) | |
| Whipple disease | |
| Cerebral malaria | |
| Encephalitis | |
| Systemic infection | |
| Inflammatory | Systemic lupus erythematosus |
| Sjögren syndrome | |
| Temporal arteritis | |
| Hashimoto encephalopathy | |
| Sydenham chorea | |
| Sarcoidosis | |
| Neoplastic | Primary or secondary cerebral neoplasm |
| Systemic neoplasm | |
| Pancreatic cancer | |
| Paraneoplastic encephalitis | |
| Endocrine/acquired metabolic | Hepatic encephalopathy |
| Uremic encephalopathy | |
| Dialysis dementia | |
| Hypo/hyperparathyroidism | |
| Hypo/hyperthyroidism | |
| Addison disease/Cushing disease | |
| Postpartum | |
| Vitamin deficiency: B12, folate, niacin, vitamin C | |
| Gastric bypass associated nutritional deficiencies | |
| Hypoglycemia | |
| Vascular | Stroke |
| Multiinfarct dementia | |
| Central nervous system vasculitis | |
| Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) | |
| Degenerative | Alzheimer disease |
| Lewy body disease | |
| Frontotemporal dementias | |
| Parkinson disease | |
| Progressive supranuclear palsy | |
| Huntington disease | |
| Corticobasal ganglionic degeneration | |
| Multisystem atrophy/striatonigral degeneration/olivopontocerebellar atrophy | |
| Idiopathic basal ganglia calcifications/Fahr disease | |
| Demyelinating/dysmyelinating | Multiple sclerosis |
| Acute disseminated encephalomyelitis | |
| Adrenoleukodystrophy | |
| Metachromatic leukodystrophy | |
| Inherited metabolic | Wilson disease |
| Tay-Sachs disease | |
| Adult neuronal ceroid lipofuscinosis | |
| Niemann-Pick type C | |
| Acute intermittent porphyria | |
| Mitochondrial encephalopathy, lactic acidosis and stroke-like episodes | |
| Epilepsy | Ictal |
| Interictal | |
| Postictal | |
| Forced normalization | |
| Post epilepsy surgery | |
| Medications | Analgesics |
| Androgens | |
| Antiarrhythmics | |
| Anticonvulsants | |
| Anticholinergics | |
| Antibiotics | |
| Antihypertensives | |
| Antineoplastic agents | |
| Corticosteroids | |
| Dopamine agonists | |
| Oral contraceptives | |
| Sedatives/hypnotics | |
| Steroids | |
| Drugs of abuse | Alcohol |
| Amphetamines | |
| Cocaine | |
| Hallucinogens | |
| Marijuana | |
| MDMA (Ecstasy) | |
| Phencyclidine | |
| Drug withdrawal syndromes | Alcohol |
| Barbiturates | |
| Benzodiazepines | |
| Amphetamines | |
| Toxins | Heavy metals |
| Inhalants | |
| Other | Normal pressure hydrocephalus |
| Ionizing radiation exposure | |
| Decompression sickness |
Stroke and Cerebral Vascular Disease
Psychosis or psychotic features may present as a rare complication of a single stroke, but the prevalence of these features is not well established. Manifestations may include paranoia, delusions, ideas of reference, hallucinations, or psychosis. Paranoia and psychosis have been reported in association with left temporal strokes that result in Wernicke aphasia. Other regions producing similar neuropsychiatric symptoms include the right temporoparietal region and the caudate nuclei. Right hemispheric lesions may also be more associated with visual hallucinations and delusions. Reduplicative paramnesia and misidentifications syndromes such as Capgras syndrome and Fregoli syndrome have also been reported. Reduplicative paramnesia is a syndrome in which patients claim that they are simultaneously in two or more locations. It has been observed to occur in patients with combined lesions of frontal and right temporal lobe but has also been described as due to temporal-limbic-frontal dysfunction (Moser et al., 1998). Capgras syndrome is the false belief that someone familiar, usually a family member or close friend, has been replaced by an identical-appearing imposter. It has been proposed that this results from right temporal-limbic-frontal disconnection resulting in a disturbance in recognizing familiar people and places (Feinberg et al., 1999). In Fregoli syndrome, the patient believes a persecutor is able to take on a variety of faces, like an actor. Psychotic episodes can also be a manifestation of complex partial seizures secondary to stroke. Patients with poststroke psychosis are more prone to have comorbid epilepsy than poststroke patients without associated psychosis. Lesions or infarcts of the ventral midbrain can result in a syndrome characterized by well-formed and complex visual hallucinations referred to as peduncular hallucinosis. Obsessive-compulsive features have also been reported with strokes. These symptoms have been postulated to be due to dysfunction in the orbitofrontal-subcortical circuitry (Saxena et al., 1998).
Consensus criteria for accurately diagnosing vascular cognitive impairments and dementia are lacking (Bowler and Gorelick, 2009; Wiederkehr et al., 2008). The vascular cognitive impairments can be conceptualized as being made up of three groups: vascular dementia, mixed vascular dementia and AD pathology, and vascular cognitive impairment not meeting criteria for dementia. These conditions may have variable contributions from mixed forms of small-vessel disease, large-vessel disease, and cardioembolic disease, which accounts for the clinical phenotypic heterogeneity. AD pathology is commonly found in association with cerebrovascular disease pathology, leading to uncertainty with respect to the relative contributions of each in some cases. A temporal relationship between a stroke and the onset of dementia or a stepwise progression of cognitive decline with evidence of cerebrovascular disease on examination and neuroimaging are considered most helpful. No specific neuroimaging profile exists that is diagnostic for pure cerebrovascular disease-related dementia. Vascular dementia may present with prominent cortical, subcortical, or mixed features. Cortical vascular dementia may manifest as unilateral sensorimotor dysfunction, abrupt onset of cognitive dysfunction and aphasia, and difficulties with planning, goal formation, organization, and abstraction. Subcortical vascular dementia often affects frontosubcortical circuitry, resulting in executive dysfunction, cognitive slowing, difficulties with abstraction, apathy, memory problems (recognition and cue recognition relatively intact), working memory impairment, and decreased ability to perform activities of daily living. Memory difficulties tend to be less severe than in AD. Limited data suggest that cholinesterase inhibitors are beneficial for treatment of vascular dementia, as demonstrated by improvements in cognition, global functioning, and performance of activities of daily living.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree