Figure 11.1 The peripheral reflex pathway
Table 11.1 Common focal peripheral nerve disorders
| Nerve | Main site | Mechanism | Main Cause | Clinical Features |
| Median | wrist | entrapment | carpal tunnel syndrome, leprosy | pain, tingling hand/wrist, arm, numbness radial 3 & 1/2 fingers, wasting thenar muscles, weakness of thumb abduction |
| Ulnar | elbow | compression | trauma/injury, leprosy | pain, tingling hand wrist, numbness ulnar 1 & 1/2 fingers, wasting hypothenar muscles, weakness little finger flexion, claw hand deformity |
| Radial Sciatic | arm buttock | compression infiltration | sleep injection | wrist drop, weakness wrist, dorsiflexion pain buttock, leg, foot, numbness leg and foot, weakness knee flexion & muscles below knee, absent ankle jerk |
| Femoral | thigh | vascular | diabetes | pain thigh (severe), numbness anteromedial thigh & medial leg, weakness hip flexion & knee extension, absent knee jerk |
| Lateral cutaneous nerve thigh | inguinal ligament | compression | occupational, carrying baby on hip | numbness, tingling and pain over anterolateral thigh (meralgia paraesthetica) |
| Common peroneal | knee | compression infiltration | illness, leprosy, leg crossing | numbness dorsum foot, foot drop, weakness foot eversion |
Table 11.2 Main causes of polyneuropathies in Africa
| Classification | Cause | Crude frequency |
| Infection | HIV, leprosy | very common |
| Metabolic | diabetes, (renal failure) | common |
| Drugs | ARTs (stavudine, didanosine), isoniazid, dapsone, vincristine | common |
| Toxic | alcohol, (chronic cassava consumption) | common |
| Deficiency | vitamin B-1 (alcoholics), B-6 (isoniazid), B-12 (pernicious anaemia) | uncommon |
| Inflammatory | Guillain-Barre Syndrome (GBS), chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) | very uncommon |
| Vasculitis | rheumatoid arthritis, systemic lupus erythematosus (SLE), polyarteritis nodosa (PAN) | uncommon |
| Hereditary | Charcot-Marie-Tooth disease, others | uncommon |
| Neoplastic paraproteinaemia paraneoplastic | monoclonal gammopathy, carcinoma lung, breast, ovary | very uncommon |
| Idiopathic (>50% of all peripheral neuropathies) | unknown | most common |
Pathophysiology
Peripheral nerves are made up of multiple axons surrounded by myelin, Schwann cells and their covering sheaths. Individual axons are either myelinated or nonmyelinated. In neuropathies the nerves may be damaged at three main sites: the axon, the myelin and the cell body. If the axon is damaged, it is called an axonal neuropathy. This is the most common form of peripheral neuropathy and usually affects sensation greater than power and has a mainly distal distribution. If the myelin is damaged this is called a demyelinating neuropathy. This affects power more than sensation and the weakness is usually proximal as well as distal. If the cell body is damaged then either sensory or motor nerve fibres or both may be damaged permanently depending on which cell body is involved. Recovery occurs if the basement membrane survives but is faster in demyelinating than in axonal neuropathies.
TYPES OF PERIPHERAL NERVE DISORDER (PND)
Peripheral neuropathies are divided into two main groups: mononeuropathies which involve single nerves and polyneuropathies which involve many nerves.
MONONEUROPATHY
This describes a group of focal peripheral nerve disorders (FPNDs) where individual nerves or their branches are affected. The main mechanisms are compression, entrapment, vasculitis, infiltration and infection. In the upper limbs, this happens mostly at the wrist, elbow and occasionally the upper arm. In the lower limbs, the most common sites are at the level of the inguinal ligament, the knee and the buttocks. A misplaced injection in the buttocks in young children is the main cause of sciatic nerve injury in Africa. If more than one nerve is involved, this is called multiple mononeuropathy or mononeuritis multiplex. Leprosy is a common cause of both mononeuropathy and mononeuritis multiplex in Africa. Other causes include HIV, diabetes and vasculitis. The main clinical features of the most common focal nerve lesions are outlined in Table 11.1 and illustrated in Figs 11.2–5.
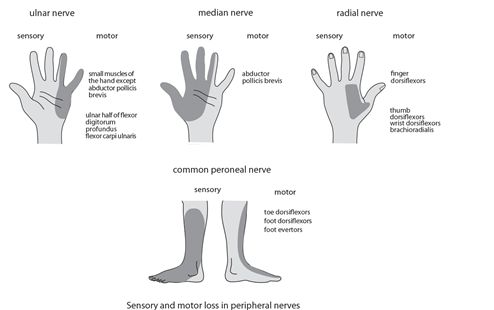
Figure 11.2 Sensory and motor loss in main mononeuropathies
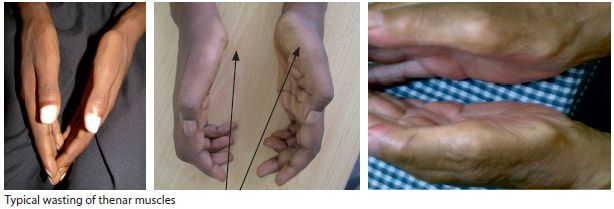
Figure 11.3 Median neuropathy (bilateral)
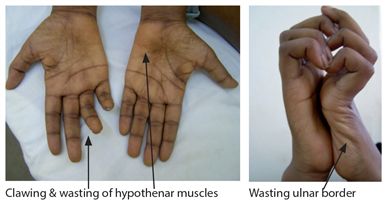
Figure 11.4 Ulnar neuropathy

Figure 11.5 Common peroneal nerve neuropathy. Bilateral foot drop (left > right)
Median nerve compression occurs mostly at the wrist as the median nerve passes through the carpal tunnel resulting in carpal tunnel syndrome (CTS). CTS is characterized by tingling pain in the hand or arm particularly at night. The pain and paraesthesiae are in the distribution of the median nerve and involve the thumb, index, middle and half the ring finger but may extend up the forearm and arm. It often wakes the patient from sleep at night and is relieved by hanging the arm down and shaking the hand. CTS is frequently provoked by manual tasks. Sensory loss in CTS usually affects the lateral (radial) three and a half fingers and spares the palm. Sensation to the lateral fingers and palm are lost in median nerve lesions located in the forearm (Fig. 11.2). In long standing cases there is wasting of the thenar eminence and weakness of thumb abduction and opposition (opponens pollicis) (Figs 11.2 & 3). Tinel’s sign may be positive i.e. tapping the carpal tunnel at the distal crease of the wrist reproduces pain and tingling. Alternatively there may be tingling on extreme wrist flexion for one minute (Phalen’s sign). However, in clinical practice these signs, although useful when present are unreliable when absent. Treatment is by local injection of steroids, wearing a night time wrist splint or by surgical decompression if necessary
Ulnar nerve is prone to compression along its path. The main site of pressure or stretching is at the elbow within the cubital tunnel or the ulnar groove. This results in dyasthesia/paraesthesia and sensory impairment/loss in the distribution of the little finger and adjacent half of the ring finger and ulnar aspect of the hand front and back. There is wasting and weakness of the intrinsic muscles of the hand and the deep flexors of the 4th and 5th finger with sparing of the thenar muscles (Figs. 11.2 & 4). This gives rise to the characteristic claw hand deformity seen in chronic ulnar lesions.
Radial nerve compression arises mostly from prolonged abnormal posture with resulting compression of the radial nerve in the radial groove above the elbow e.g. drunkard’s palsy. It can also arise from compression in the axilla, e.g. using crutches, and from fracture of the shaft of the humerus. Compression results in wrist drop with weakness of the finger and wrist extension and sometimes a small patch of sensory loss on the dorsum of the hand and web of the thumb (Fig. 11.2).
Lateral cutaneous nerve of thigh travels under the lateral part of the inguinal ligament. Compression results in a patch of sensory loss over the anterolateral aspect of the thigh of variable size ranging from a palm sized patch to an area extending from the hip to the knee but never crossing the midline of the axis of the thigh (meralgia paraesthetica). This is one of the most common mononeuropathies and its onset is associated with weight gain e.g. pregnancy and also occupational e.g. chronic abnormal posture, bending (e.g. plumber). It is usually self-limiting.
Sciatic nerve injury most commonly occurs as a result of a misplaced injection in the buttocks in early childhood. The sciatic nerve (tibial & common peroneal nerves, L4,5,S1,2) is responsible for sensation below the knee involving the entire anterolateral aspect of leg and the sole and dorsum of the foot. It is responsible for the following movements, hip extension, knee flexion and ankle plantar and dorsiflexion. Injury results in loss of sensation and power in these distributions along with a decreased or absent ankle jerk.
Common peroneal nerve compression at the fibular head results in foot drop and sensory loss on the dorsum of foot and lateral leg (Figs 11.2 & 5). The main causes are trauma and pressure. It occurs more commonly in immobile patients who are prone to compression.
Femoral neuropathy most commonly occurs in association with diabetes mellitus. The main symptoms are thigh pain, weakness of hip flexion and decreased or absent knee jerk. Treatment is pain relief and treating the underlying cause.
Key points
- mononeuropathies are recognised by their clinical setting & pattern of sensory & motor loss
- include CTS: ulnar injury, peroneal palsy, meralgia paraesthetica, sciatic injury & femoral ischaemia
- main mechanisms: trauma, entrapment, compression, infection & inflammation
- leprosy is a major cause of mononeuropathies
- a misplaced injection is main cause of sciatic nerve injury
POLYNEUROPATHIES
Polyneuropathies are diffuse, symmetrical disorders usually affecting the limbs distally to a greater extent than proximally. Clinically, they are classified as acute or chronic, motor or sensory or mixed and also autonomic. Patients presenting with polyneuropathies typically present with impairment or loss of sensation in a distal or peripheral glove and stocking distribution. Distal weakness may occur later in the feet and legs followed by the hands and arms. Neurological examination usually reveals wasting, fasciculation, distal weakness with absent reflexes and loss of light touch. Vibration and joint position sense may also be involved. The sphincters involving bowel and bladder are typically spared. The main causes of polyneuropathy are outlined in Table 11.2.
Main causes of polyneuropathy in Africa
- HIV
- diabetes
- leprosy
- drugs
- alcohol
- nutrition
Clinical features
The history may provide the first clue as to the aetiology of a neuropathy. There may be a history of a known risk factor for neuropathy, e.g. HIV, use of antiretroviral drugs (ART) in particular stavudine, diabetes, alcohol abuse, renal failure or very rarely a family history. The history provides essential information concerning the mode of onset, time course, distribution, character and pattern of symptoms.
The clinical distribution will indicate whether it is confined to just one nerve or is more generalised affecting all peripheral nerves. An acute onset over days with both proximal and distal weakness suggests a demyelinating disorder like GBS, whereas a more chronic onset over months suggests a distal sensory motor axonal neuropathy as occurs in DM or HIV. Burning or pain in the feet is very characteristic of the neuropathy in HIV, diabetes, vitamin deficiencies and alcoholism. Additional clinical findings may also indicate the cause; the peripheral nerves may be thickened in leprosy, or clawing of the feet or pes cavus is seen in hereditary neuropathies or the low blood pressure on standing characteristic of autonomic neuropathies. The predominance of either sensory or motor findings is also helpful.
Motor
Muscle weakness suggests motor neuropathy. Motor symptoms include mild to severe weakness in the limbs, problems with walking or running, and difficulties manipulating or using fingers and hands. The main causes of motor neuropathy are GBS, polio and very rarely lead poisoning. Main findings on neurological examination include wasting, weakness and loss of reflexes in the limbs (Fig.11.6).

Figure 11.6 Motor and sensory neuropathy
Sensory
Numbness, tingling or pain in a glove and stocking distribution suggest a mainly sensory neuropathy. Terms used to describe the superficial sensory symptoms include: paraesthesia, meaning abnormal tingling sensation; hyperaesthesia, meaning increased sensitivity to a stimulus and dysaesthesia, meaning unpleasant tingling. The term allodynia means painful sensation from light non painful stimulus e.g. stroking. Sensory symptoms tend to occur before motor symptoms and typically involve the feet earlier than hands. Findings on neurological examination include loss of light touch, pain and joint position sense distally in the limbs mostly the feet. A sensory polyneuropathy may also cause poor balance and unsteady gait due to a loss of position sense in the feet. This is called sensory ataxic neuropathy. When the neuropathy involves loss of pain then trophic changes and digital loss can occur (Fig. 11.7)

Figure 11.7 Sensory neuropathy
Differential Diagnosis
The differential diagnosis of neuropathies includes diseases affecting muscle, neuromuscular junction and occasionally myelopathy and rarely motor neurone disease. Polymyositis and myopathy may sometimes mimic a neuropathy but skin involvement and the mainly proximal pattern of weakness should suggest underlying muscle disease. Fatigability after exercise, a mainly truncal-axial pattern of weakness, ptosis and intact reflexes all point to myasthenia gravis. While myelopathy symptoms may sometimes mimic neuropathy, the predominantly upper motor neurone signs, the sphincteric involvement and pattern of sensory loss or alteration should all suggest spinal cord involvement. Exclusive motor involvement with weakness and fasciculation are pointers towards progressive muscular atrophy (PMA), a form of motor neurone disease, although this is uncommon.
Diagnosis
The diagnosis of peripheral neuropathy relies mainly on the clinical findings and in as many as half the cases no underlying cause is found. Investigations should include laboratory screening tests for the common causes as outlined in Table 11.3. Simple blood tests exclude causes such as HIV, diabetes and B-12 deficiency. CSF examination may show an elevated protein in GBS and CIDP. Nerve conduction studies and electromyography are very helpful if available.
Table 11.3 Laboratory investigations in peripheral neuropathy
| Type Haematology | Investigation FBC, B-12, folate, HIV, VDRL, ESR | Disorder vit deficiency, HIV, syphilis infection, vasculitis |
| Biochemistry | glucose, renal, liver, thyroid function tests, protein electrophoresis | diabetes, renal failure, myxoedema, paraproteinaemia |
| Urine | cells, protein casts | |
| Immunology | auto antibodies: ANCA, rheumatoid factor, antinuclear antibody | RA, SLE, PAN |
| X-ray | chest, bones | malignancy, myeloma |
| Lumbar puncture | protein | GBS, CIDP |
| Electrical | NCS | axonal versus demyelinating |
| Skin slit smears/biopsy | acid fast bacilli | leprosy |
Nerve conduction studies (NCS) and Electromyography (EMG)
These are used mainly to determine whether there is a disease of the peripheral nerves, neuromuscular junction or muscle and to distinguish between them. NCS can also determine whether the neuropathy is purely sensory or also affects the motor fibres and whether the primary disease is axonal (causing death of axons) or demyelinating (affecting Schwann cells and myelin sheaths) or a mixture of both.
NCS involve stimulating a nerve with an electrical impulse and measuring the speed of conduction at two points along the nerve. This is called the conduction velocity. NCS also involves recording and measuring the amplitude of muscle action potential (MAP). NCS can distinguish demyelinating from axonal neuropathies. In general, a reduction in conduction velocity and normal MAP favours demyelination whereas normal conduction velocity and reduced MAP favours axonal neuropathies. Most neuropathies are axonal in type and largely untreatable. The most common type is termed distal symmetrical polyneuropathy (DM and HIV). In contrast demyelinating neuropathies (GBS) are uncommon but are largely treatable.
EMG involves insertion of a needle electrode into muscle and measures electrical activity in muscles. The patterns of electrical recordings at rest and during activity can determine the likely origin of the disorder.
Management of neuropathy
The first principle of management is to diagnose and treat the underlying cause of neuropathy. High dose corticosteroids are used in neuropathies complicating vasculitis and chronic inflammation. Other forms of immunosuppression include intravenous immunoglobulin (IVIG) and plasma exchange (PE). These are used in GBS but these are unavailable to all but the largest medical centres in Africa. Pain is controlled by local and general measures. Local measures include application of heat, and topical anaesthetics. General measures include analgesics, anti inflammatories, tricyclics, the antiepileptic drugs carbamazepine, pregabalin and gabapentin and also opiates (Chapter 20). Weak or paralysed limbs may be assisted with orthoses. General advice is given to prevent ulcers by wearing protective foot wear and avoiding injury. The most common or important individual neuropathies are presented below.
Key points
- main causes of neuropathy are HIV, diabetes, leprosy & ART
- history and examination provide clues to diagnosis & aetiology
- neuropathies are either sensory or motor or a mixture of both
- investigations involves bloods, csf examination and X-rays
- main aim is treat the underlying cause & to control symptoms
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








