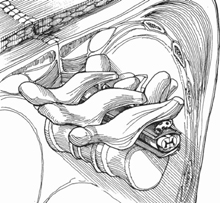
80 Milan G. Mody and Laurence D. Rhines Incidental or inadvertent durotomies are infrequent (4 to 14% incidence) but serious complications in spinal surgery. Several intra- and postoperative surgical strategies are available for proper and timely management of cerebrospinal fluid (CSF) leaks. Timely effective strategies for controlling CSF leaks can lead to good clinical outcomes and avoid serious sequelae such as postural headaches, pseudomeningocele, meningitis, durocutaneous fistulas, epidural abscess, and persistent neuropathy. These techniques can provide stable control of CSF egress from incidental durotomy. The gold standard for treatment of all CSF leaks is primary repair of the dural defect with 5-0 or 6-0 Prolene or Neurilon. There are certain pathologic situations and intraspinal locations for which primary repair may be technically formidable or impossible and require patch techniques (Fig. 80.1). This includes a durotomy in the setting of anterior cervical or lumbar diskectomy, en bloc removal of tumor with adherent dura, resection of an intradural tumor, microdiskectomy with adherent nerve root sleeve, adherent stenotic ossification of the posterior longitudinal ligament (OPLL) or ligamentum flavum, and traumatic bony laceration of dura. Fig. 80.1 Type A tear can be repaired primarily, whereas type B opening requires patch technique. Types C and D tears should be considered for fat, fibrin glue, or collagen matrix onlay bailout. Do not attempt primary dural repair if under tension secondary to a large defect or constraining adhesions. Pinhole high-pressure leaks are better treated with enlargement and primary suture closure. A patch repair cannot be performed if a dural edge cannot be circumferentially exposed. Management of durotomy in the setting of an acute infection is a challenge. There is a published association of dural tears with smoking, diabetes, more than three epidural steroid injections 6 months prior to surgery, trauma, and revision surgery. Preoperative planning enables the surgeon to be prepared for dural repair with a choice of graft. Patients must be informed of the nature, purpose, risks, benefits, and alternatives of autograft (fascia lata, lumbodorsal fascia, or fat), allograft (cadaveric dura or pericardium), xenograft (bovine pericardium), or synthetic (Gore-Tex or DuraGen [Integra Life Sciences Corp., Plainsboro, NJ] collagen matrix suture or sutureless) patch grafts. A surgical microscope or loupes can enhance the evaluation and repair of durotomies. The availability of specialized instruments such a watchmaker’s or knot-tying forceps, microscissors, microneedle holder, and knot-pusher can mitigate the technical difficulty of a small workspace. If autograft fascia lata is to be used for patch repair, then the patient’s lateral thigh should be available, prepped, and draped at the start of the procedure. Anesthesia personnel will have to perform Valsalva maneuver to test the repair or sometimes identify the pinhole tear. Local erector spinae fascia or fat is readily available without increased risks. Collagen matrix onlay can be successful with limited technical or time demands but adds to material costs. Autograft fascia lata has the best handling characteristics and does not pose the risk of disease transmission but requires separate incision with associated morbidity including possible weakness of leg abduction. Placement of an intradural lumbar drain for 3 to 5 days reduces CSF pressure on the repair; however, the surgical and nursing staff must be extremely diligent in monitoring the flow (<10 cc/hr) and position (ear or shoulder level). Remember to continue prophylactic antibiotics until the drain is discontinued. If CSF appears cloudy or turbid, then fluid should be sent for Gram stain and cultures. We recommend placing a skin stitch upon drain removal to minimize leakage. If there is persistent drain-site leakage, then place a pressure dressing and institute bed rest for 2 to 3 more days. Some authors have wisely advised that we label these events as “intraoperative dural openings” and drop the medicolegal-laden terms such as “inadvertent or incidental durotomy or dural tears.” If using DuraGen collagen matrix onlay (sutureless) technique, then a local drain is required (Fig. 80.2). With other techniques, however, local drains may pose the risk of repair breakdown or encourage formation of CSF fistula. If a local drain is preferred, then we recommend draining off the suction. Although a Gore-Tex synthetic graft is readily available, it is relatively stiff and requires special needles and suture, which makes it challenging in a narrow workspace. Patch suturing does leave pinholes from the suture needle that can be sealed with fibrin glue.
Dural Repair and Patch Techniques: Anterior and Posterior
Description
Key Principles
Expectations
Indications

Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







