16 Endoscopic Periorbital and Optic Nerve Surgery and Intraorbital Resections
Richard J. Harvey, Raymond Sacks, Aldo Cassol Stamm, and João Flávio Nogueira
 Introduction
Introduction
External approaches to the orbit are essential in managing pathology lateral to the optic nerve and globe (the neural axis). For those lesions that are medial to the neural axis or displace the neural structures laterally, endoscopic approaches offer an incision-free approach. Additionally, there is preservation of sinonasal physiology in the approach for orbital and periorbital pathology. Endoscopic approaches also include endoscopic-assisted transcaruncular, transconjunctival1,2 (to the floor), transblepharoplasty3 (to the roof) approaches to the orbit, and transsupraorbital craniotomy.4 However, this chapter focuses on the endoscopic transnasal/ sinus surgery.
Endoscopic techniques rely on the presence of an operative cavity in which to work. Distensible spaces are created in laparoscopic surgery, and, similarly, sinus cavities provide the operative field in sinus surgery. However, the intraorbital fat precludes easy operative working space in the orbit. Distension of the intraconal tissues is limited due to the bony confines of the orbit. Although lateral orbitotomy can be performed to allow temporary lateral shift of intraorbital structures,5 significant limitations remain in the ability to create a working space within orbital fat.
Utilizing the maxillary, ethmoid, and sphenoid sinuses to define the orbital axis and create a working space is a fundamental part of our endoscopic orbital surgery (Fig. 16.1). Further subperiosteal (subperiorbital) dissection can occur both superior and inferior around the orbital contents to access pathology. Once the periorbita is opened, however, prior displacement of orbital fat by pathology is important to have a workable operative field. Orbital fat can be displaced, removed, or ablated to reach pathology, but the conal muscles and neurovascular structures within the orbit make this a challenging exercise. The lack of dead space due to the inter-muscular septations and ubiquitous fat will always obscure visualization if not previously displaced.
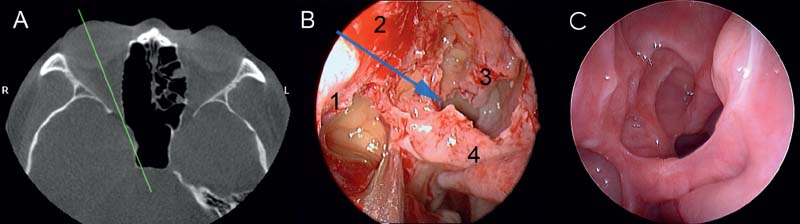
Fig. 16.1 The orbital axis. Defining the line of the orbit in endoscopic surgery is important (A,B). It also allows easy postoperative surveillance (C).
 Indications and Advantages
Indications and Advantages
Posterior access to pathology near the orbital apex is excellent via an endoscopic approach. The near vision view allows easy identification of the optic nerve transition to the orbit apex and fibrous annulus. Endoscopic approaches also avoid disruption of the orbicularis oculi, lacrimal pump, or canthal ligament disruption. The final access to any orbital pathology will ultimately need to be customized to the patient and the lesion. However, the final goal should always be to preserve ocular function and effectively treat the pathology. The combined efforts of both the ophthalmologist and the rhinologist are essential to ensure an optimal outcome for extended endoscopic orbital surgery.5–7
A summary of common indications for endoscopic orbital surgery is presented below. Thyroid eye disease and inflammatory conditions, such as subperiosteal abscess, are not discussed in this chapter.8,9 However, the surgical management of these lesions utilizes the same principles discussed for managing more extended pathology. Absolute contraindications to the endoscopic approach are pathology lateral to the neural axis and a lack of specialized equipment and expertise. A relative contraindication is the presence of acute or subacute sinusitis. These conditions should be managed medically if possible prior to any intervention. Chronic rhinosinusitis is not a contraindication, as many of the persistent mucosal changes in this condition are inflammatory rather than infective. Chronic mucosal disease is often present in managing these lesions because sinonasal dysfunction often occurs from the local effects of large masses.
Common Indications
Extraconal Pathology
Neoplastic
Meningioma10
Osteoma11
Inverted papilloma12
Solitary fibrous tumor13
Malignant disease14
Chondrosarcoma
Optic nerve trauma (sheath excision)15–17
Fibro-osseous18
Intraconal Pathology
Schwannoma
Removal of foreign body21
 Diagnostic Workup
Diagnostic Workup
Radiologic Assessment
Orbital evaluation is based on the combination of magnetic resonance imaging (MRI) and computed tomography (CT). The use of fat-suppression sequences in MRI greatly assists delineation of intraorbital pathology.
Ophthalmology Assessment
Formal visual acuity and visual field assessment is required to delineate any deficit, including papilledema. Formal visual assessment is performed with an ophthalmologist. Other cranial neuropathies need to be documented.
 Surgery
Surgery
Instruments
There are several instruments beyond the standard endoscopic sinus surgery setup that are required to manage orbital pathology. These include a diamond burr; a bipolar, sharp right-angle knife; and suction dissection elevator.
The diamond burr is essential for three areas. First, the junction of the medial orbital wall to the lateral wall of the sphenoid results in a thick buttress of bone (optic tubercle22). Controlled removal of bone and subsequent exposure of the optic canal in the lateral sphenoid wall is required. The optic canal is too narrow for rongeurs to be used for bone removal. Second, the medial orbital wall is commonly too thick to simply fracture and discover the periorbita. Thinning down of the bone prior to removal is important to preserve the periorbita and allow further dissection. Small amounts of fat exposed into the surgical field will have little functional significance but dramatically change the conditions of the surgical field. Fat protruding will obscure the view and increase the chance of further trauma from instruments (drills/ debriders). Third, the bone around the upper lacrimal sac is often too thick to be removed with a rongeur alone. Full exposure of the lacrimal apparatus is often required in both access and reconstruction during orbital surgery.
The bipolar forceps is essential to control intraorbital vessels, especially the anterior and posterior ethmoidal arteries and control periorbital vasculature. Standard neurosurgical bayonets are often not appropriate via the long surgical corridor of endoscopic skull base surgery. Specialized bipolar instrumentation is essential. The availability of hemostatic materials and techniques are important, but the principles of hemostasis in endoscopic surgery differ little from those of open surgery. Prevention of bleeding is obviously the best solution. Tumor debulking, extracapsular sharp dissection, and countertraction using gentle suction still form the foundation of vascular control.23
Carefully incising the periorbita, lacrimal sac, or optic nerve sheath requires a sharp blade. Simple nasal sickle knives are often not sufficient, and No. 11 surgical blades may be too big and not allow enough freedom of movement to make angled cuts. Straight and right-angled keratome blades, dedicated dacrocystorhinostomy (DCR) blades, or beaver blades are usually required. Finally, dissection in the subperiosteal space of the orbita is often facilitated by a suction or malleable suction dissector. As the periorbita is elevated, the exposed bony haversian channels initially provide a bloody narrow surgical field that will eventually resolve. Suction instruments can be of value in the initial elevation.
Preparation
Endoscopic transnasal craniotomy is performed under general controlled hypotensive anesthesia without Mayfield fixation. Total intravenous anesthesia is associated with better mucosal hemostasis.24,25 Cotton pledgets containing adrenaline 1:1000 are placed in the nasal cavity over the areas of surgical access for 10 minutes before the surgical procedure. The lateral nasal wall and septum are infiltrated with 1% Naropin with adrenaline 1:100.000.
Approach
Extraconal Lesions
An uncinectomy, wide antrostomy combined with anterior and posterior ethmoidectomy is performed. The antrostomy is widened superiorly to ensure that the maxillary sinus roof can be easily seen. This defines the orbital floor, allows easier skeletonization of the medial orbital wall, places the infraorbital canal on view, and is an important landmark for defining the level of the skull base posteriorly. A parallel line to the nasal floor from the maxillary sinus roof facilitates safe debulking of tumor and access to the sphenoid sinus (Fig. 16.2). The inferior half of the superior turbinate is resected to give access to the entire front wall of the sphenoid. The maximum amount of the front wall is then removed by commencing at the sphenoid ostium. The sphenoid sinus is key for orientation, as the roof defines the skull base and the lateral wall defines the optic nerve canal.
Prior to any pathology removal, the full axis of the orbit is usually defined (Fig. 16.1). Division of the sphenopalatine artery may be required to assist with hemostasis. Additional access to the orbital floor can be achieved using further access routes. A maxillary trephine through the intersection of the midpupillary point and the transverse line extending from the nasal sill allow an additional port for an endoscope or other instrument. Dental or anterior superior alveolar nerve injury is minimal using these landmarks.26–28 The modified medial maxillectomy29 was originally described to manage recalcitrant inflammatory disease30,31 but has become a useful technique to increase access to the maxillary sinus and orbital floor.
Access above the orbital contents and the bony roof of the orbit is limited by the frontoethmoidal suture line and the neurovascular structures traversing it.32 The anterior and posterior ethmoidal arteries need to be exposed either from their bony canal (Fig. 16.3) or on the orbital side to allow further lateral dissection on the orbital roof.33
Involvement of the Lacrimal System by Tumor
Anteriorly, orbital pathology may involve the lacrimal system. Depending on the extent of the involvement of the lacrimal system by the tumor, various reconstructive options are available. When tumor involves nasolacrimal duct, the duct can be completely resected along with the tumor and typically no formal reconstruction is required. After the surgical margin is defined, the remaining duct can simply be marsupialized. Should the remaining duct be less than 5 mm, then a formal DCR is preferred (Fig. 16.4A). For tumor involving the lacrimal sac, a formal endoscopic DCR with wide bone removal is required. The medial sac wall can be safely sacrificed and the DCR completed as per standard techniques. Occasionally the lateral sac mucosa will need to be resected, and reconstruction will need to be achieved by the placement of a free mucosal graft. A 3-mm punch biopsy cutter is used on a Blakesley forceps to preserve the common canaliculus opening and mucosa. The remaining lateral sac is removed. A central perforation of the graft is created with the same 3-mm punch biopsy instrument. The graft is placed to provide nearly complete mucosal apposition, preserving the common canaliculus. Stenting is used, and then a Gelfoam “donut” dressing is used to secure the graft (Fig. 16.4B). Finally, when a tumor involves the common canaliculus, the entire sac and common canaliculus need to be resected, and reconstruction will be required by the insertion of a glass Jones tube through the medial canthus (Fig. 16.4C). This is best performed in combination with an ocular plastic surgeon and an endoscopic surgeon.
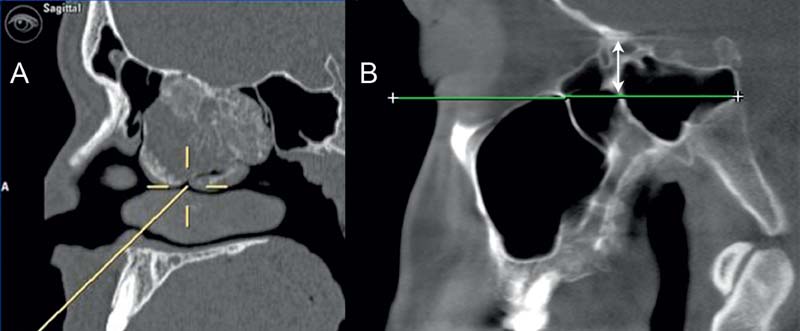
Fig. 16.2 The orbital floor. (A) Intraoperative orientation is important with large pathology such as this chondrosarcoma of the ethmoid. (B) A line from the maxillary sinus roof (parallel with reference to the nasal floor) enables safe identification of the skull base posteriorly and provides an entry to the sphenoid sinus. Discovery of the entire lateral sphenoid wall in orbital surgery is essential.




