25 Endoscopic Transnasal Pituitary Surgery
Aldo Cassol Stamm, Eduardo Vellutini, Daniel Timperley, and Leonardo Balsalobre
 Introduction
Introduction
Endoscopic pituitary surgery (EPS) is a well-established technique for the treatment of sellar tumors, especially pituitary adenomas. It offers some advantages compared with microscopic approaches, such as a superior close-up view of the relevant anatomy, an enlarged working angle, and increased panoramic vision inside the surgical area.1–4
Several studies, including a large systematic review, show that EPS decreases the operating time, the use of lumbar drains, the risk of postoperative diabetes insipidus, the length of hospital stay, patient discomfort, and rhinologic complications.1–6
The pituitary gland is well accessed through the nasal cavity and sphenoid sinus, and since the last century several approaches have been described.
This chapter discusses techniques that can improve the results in pituitary surgery, with more radical removal, optic chiasm decompression, and better endocrinologic results.
Pituitary surgery can be divided into nasal, sellar, and reconstructive stages. The nasal stage provides access to the sphenoid sinus via various approaches and is discussed in more depth in Chapter 14. The sellar stage is the main focus of this chapter, and the reconstructive options are discussed briefly.
 Nasal Stage
Nasal Stage
Adequate exposure of the sphenoid sinus is essential. In addition to maximizing the lateral extent of the sphenoidotomy, lowering the opening to the floor of the sinus is important to provide access to the inferior aspect of the sella. The panoramic view possible with the endoscope enables visualization of anatomic landmarks, which aids surgical orientation (Fig. 25.1). A wide opening into the sphenoid also enhances the ability of two surgeons to operate simultaneously without the crowding of instruments, enabling sharp capsular dissection and improving the ability to control bleeding. Small openings restrict both visualization and the number of instruments that can be used simultaneously, resulting in reliance on curettage and blind scraping techniques with limited ability to manage bleeding.7 The various approaches are discussed in Chapter 14.
 Sellar Stage
Sellar Stage
The sellar stage of the procedure begins with the identification of landmarks through the wide sphenoidotomy created during the nasal stage. A panoramic view should be obtained, enabling bilateral identification of the opticocarotid recesses, internal carotid arteries, and optic nerves in one view of the endoscope. The sella, clivus, and planum are identified in the midline (Fig. 25.1).
The intersinus septum and accessory septa are removed. Particular care is taken where a septum is attached over the carotid artery to avoid an uncontrolled fracture, which may result in arterial injury. The sphenoid mucosa is displaced laterally, rather than stripping the lining of the sinus. Bleeding from exposed bone is reduced, and the mucosa can be used to supplement sella reconstruction.
The bone of the sella is thinned using a diamond drill, or if thin, gently fractured. A Kerrison rongeur is then used to remove the bone in an extradural manner. Bone removal continues until the “four blues” are identified: the cavernous sinuses on each side and the superior and inferior intercavernous sinuses. A rectangular dural opening is then made just inside these vascular boundaries (Fig. 25.2).
After exposure of the tumor, tumor fragments are sent for pathologic examination. Excision is performed using microsurgical techniques to separate the tumor from the normal gland and sellar walls. Capsular dissection of the tumor is favored as opposed to curettage and scraping techniques. Dissection in the plane between the tumor and normal structures facilitates complete tumor removal with maximal preservation of normal tissues, particularly residual pituitary gland. For larger tumors, initial debulking is required so that the tumor collapses and dissection of the capsule is possible (Fig. 25.2). In macroadenomas, tumor resection is not complete until the arachnoid membrane of the diaphragma is identified and separated from the lesion (Fig. 25.2). Although dissection is most safely performed using a 0-degree endoscope, a 45-degree endoscope is useful to check the completeness of the resection, particularly laterally around the carotids and cavernous sinus. Venous bleeding from the cavernous or intercavernous sinuses is controlled with hemostatic materials, compression, and patience.
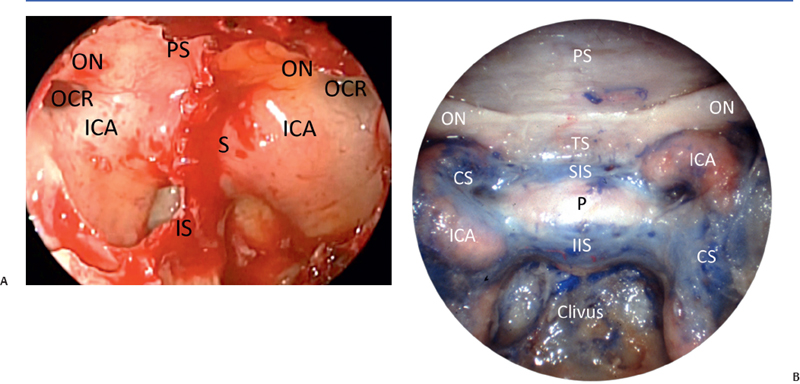
Fig. 25.1 (A) Endoscopic view of the sphenoid sinuses. A wide view of the anatomic structures facilitates surgical orientation. (B) Cadaver dissection demonstrating the position of the venous sinuses. C: clivus; ICA: internal carotid arteries; IIS: inferior intercavernous sinus; IS: intersinus septum; OCR: opticocarotid recess; ON: optic nerve; PS: planum sphenoidale; S: sella turcica; SIS; superior intercavernous sinus.




