Essential Tremor
Elan D. Louis
INTRODUCTION
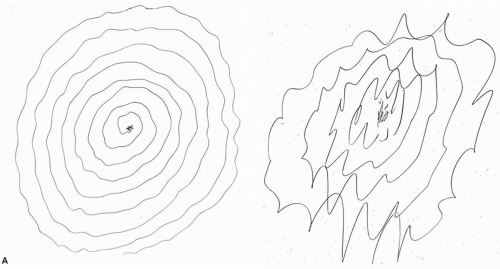
Essential tremor (ET) is a chronic, progressive neurologic disease. The hallmark motor feature is a 4- to 12-Hz kinetic tremor (tremor occurring during voluntary movements, such as writing or eating) that involves the arms and hands (Fig. 73.1). Tremor may eventually spread to involve the head (i.e., the neck), voice, and jaw. Given the presence of etiologic, clinical, and pharmacologic response profile and pathologic heterogeneity, there is growing support for the notion that ET may be a family of diseases whose central defining feature is kinetic tremor of the arms and which might more accurately be referred to as the essential tremors.
EPIDEMIOLOGY
ET is among the most prevalent adult-onset movement disorders, although it may occur at any age, and pediatric cases, with age of onset in the first decade of life, have been reported. In a recent meta-analysis of data from 28 population-based prevalence studies in 19 countries, the pooled prevalence of ET across all ages was 0.9%. The prevalence increases markedly with age and especially with advanced age. In the meta-analysis, prevalence among persons aged 65 years and older was 4.6%, and in some studies, the prevalence among persons aged 95 years and older reached values in excess of 20%. The rate at which new ET cases arise (i.e., the incidence rate) has been estimated as 619 per 100,000 person-years among individuals age 65 years and older; this incidence rises with age. Established risk factors for ET include older age and family history of ET.
ETIOLOGY
Both genetic and environmental (i.e., toxic) factors are likely contributors to disease etiology. Many large kindreds show an autosomal dominant pattern of inheritance, and first-degree relatives of ET patients are approximately 5 times more likely to develop the disease than are members of the population and 10 times more likely if the proband’s tremor began at an early age.
The prevalence of a family history of ET is high in ET patients seen in neurologic clinics and even higher in younger onset than older onset ET cases. A variant in the Lingo-1 gene has been most consistently associated with ET; however, no major causal genes have been identified so far, and this is likely due to phenocopies, incomplete penetrance, bilineal inheritance, or possibly other modes of inheritance. The existence of sporadic cases (i.e., cases without apparent family history), variability in age at onset in familial cases, and lack of complete disease concordance in monozygotic twins all argue for nongenetic (i.e., environmental) causes as well. A number of environmental toxins are under investigation, including β-carboline alkaloids (e.g., harmane, a dietary toxin) and lead. One epidemiologic study indicated a possible protective role of cigarette smoking and another suggested that higher levels of premorbid ethanol consumption raise the risk of developing ET with the presumed mechanism being Purkinje cell toxicity. The identification of modifiable risk factors would have important implications in terms of disease prevention.
The prevalence of a family history of ET is high in ET patients seen in neurologic clinics and even higher in younger onset than older onset ET cases. A variant in the Lingo-1 gene has been most consistently associated with ET; however, no major causal genes have been identified so far, and this is likely due to phenocopies, incomplete penetrance, bilineal inheritance, or possibly other modes of inheritance. The existence of sporadic cases (i.e., cases without apparent family history), variability in age at onset in familial cases, and lack of complete disease concordance in monozygotic twins all argue for nongenetic (i.e., environmental) causes as well. A number of environmental toxins are under investigation, including β-carboline alkaloids (e.g., harmane, a dietary toxin) and lead. One epidemiologic study indicated a possible protective role of cigarette smoking and another suggested that higher levels of premorbid ethanol consumption raise the risk of developing ET with the presumed mechanism being Purkinje cell toxicity. The identification of modifiable risk factors would have important implications in terms of disease prevention.
PATHOBIOLOGY
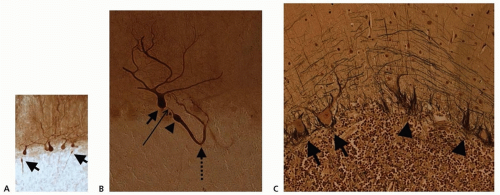
The olivary model of ET, first proposed in the early 1970s, posited that a tremor pacemaker in the inferior olivary nucleus was driving the tremor in ET. However, there are major problems with this model, including the absence of direct empirical support and, therefore, there has been trend to move away from this model. In more recent years, mechanistic research on ET has focused more on the cerebellum and the role it seems to play in the biology of ET. Interest in the cerebellum was initially motivated by neuroimaging studies, which strongly implicate the importance of this brain region in ET, and clinical studies, which frequently note the presence of cerebellar signs in patients with ET. More recently, controlled postmortem studies have revealed an array of degenerative changes in the cerebellar cortex, primarily involving the Purkinje cells and surrounding neuronal populations, in the majority of ET cases (Fig. 73.2). In some studies, there is actual Purkinje cell loss. A smaller group of ET cases demonstrates a pattern of Lewy bodies that are relatively restricted to the locus ceruleus. Of mechanistic interest is that the noradrenergic neurons of the locus ceruleus project to the cerebellum and synapse with Purkinje cells. Hence, there is growing support for the notion that the cerebellum may be central to disease pathobiology and that the pathobiology is neurodegenerative.
CLINICAL MANIFESTATIONS
Symptoms and signs of ET can begin at any age, and about 5% begin in childhood, although the incidence increases markedly with advancing age, and most prevalent cases are age 60 years or older.
The cardinal feature of ET is kinetic tremor, evidenced during a variety of activities on neurologic examination (e.g., finger-nose-finger maneuver, spiral drawing) (Video 73.1). The tremor is generally mildly asymmetric, affecting one arm more than the other, with on average an approximate 30% difference between sides; in approximately 5% of patients, the tremor is markedly asymmetric or even unilateral. In approximately 50% of patients, the tremor has an intentional component, worsening on finger-nose-finger maneuver as the patient approaches the target. Intention tremor is not limited
to the arms; in 10% of patients, it is detectable in the head when the patient’s head approaches a target (e.g., while drinking from a cup or a spoon). Postural tremor also occurs in patients with ET and is generally worse in the wing-beat position than when the arms are held straight in front of the patient. The tremor in the two arms is generally out of phase, creating a seesaw effect when the arms are held in a wing-beat position and contributing to the observation that functionality may improve when two rather than one hand is used (e.g., while holding a cup). The postural tremor of ET is generally greatest in amplitude at the wrist joint rather than more proximal or distal joints and generally involves wrist flexion extension rather than wrist rotation supination. As a rule, the amplitude of kinetic tremor exceeds that of postural tremor, and the converse pattern should raise questions about the diagnosis. Tremor at rest, without other cardinal features of parkinsonism, occurs in approximately 20% of patients with ET attending a specialty clinic, but in contrast to that of Parkinson disease (PD), it is a late feature and it has only been observed in the arm rather than the arm and leg. Another motor feature of ET, aside from tremor, is gait ataxia, which is in excess of that seen in similarly aged controls. In most patients, this is mild, although in some, it may be of moderate severity. There is some evidence that gait ataxia is more pronounced in patients with midline cranial tremors (e.g., neck, jaw, voice). Saccadic eye movement abnormalities have also been detected in ET patients in several physiologic studies, although these are of a subclinical nature.
to the arms; in 10% of patients, it is detectable in the head when the patient’s head approaches a target (e.g., while drinking from a cup or a spoon). Postural tremor also occurs in patients with ET and is generally worse in the wing-beat position than when the arms are held straight in front of the patient. The tremor in the two arms is generally out of phase, creating a seesaw effect when the arms are held in a wing-beat position and contributing to the observation that functionality may improve when two rather than one hand is used (e.g., while holding a cup). The postural tremor of ET is generally greatest in amplitude at the wrist joint rather than more proximal or distal joints and generally involves wrist flexion extension rather than wrist rotation supination. As a rule, the amplitude of kinetic tremor exceeds that of postural tremor, and the converse pattern should raise questions about the diagnosis. Tremor at rest, without other cardinal features of parkinsonism, occurs in approximately 20% of patients with ET attending a specialty clinic, but in contrast to that of Parkinson disease (PD), it is a late feature and it has only been observed in the arm rather than the arm and leg. Another motor feature of ET, aside from tremor, is gait ataxia, which is in excess of that seen in similarly aged controls. In most patients, this is mild, although in some, it may be of moderate severity. There is some evidence that gait ataxia is more pronounced in patients with midline cranial tremors (e.g., neck, jaw, voice). Saccadic eye movement abnormalities have also been detected in ET patients in several physiologic studies, although these are of a subclinical nature.
Recent years have witnessed an increasing appreciation of the presence of nonmotor features in ET patients, which may broadly be classed into cognitive, psychiatric, and sensory. Cognitive changes are in excess of those seen in similarly aged controls and range from mild changes across several domains, but especially executive function, to mild cognitive impairment and dementia, both of which occur to a greater extent than in age-matched controls. The pathobiology of these cognitive changes is unclear at present. Psychiatric manifestations include secondary anxiety and depression. The presence of a primary mood disturbance, which precedes the motor manifestations, is supported by at least one prospective study. A harm avoidant personality has been reported in studies that have assessed personality traits in ET, and this may be one feature, which makes patients reluctant to undergo therapeutic surgery even in the setting of severe and disabling tremor. Sensory changes include diminished hearing in excess of that seen in age-matched controls and a mild olfactory deficit in some although not all studies.
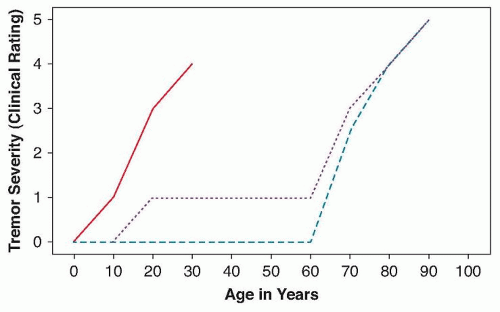
Initially, the tremor may be mild and asymptomatic and it may not worsen for years, but in most individuals, the tremor worsens over time. Several patterns of progression have been described (Fig. 73.3). The two most common are (1) late life onset and (2) early life onset with mild, stable tremor for many years and then a late life worsening. The least common pattern is that of early life onset with marked worsening over the ensuing years to decade. There are few prospective, longitudinal natural history studies, but the best estimates of rate of change indicate that arm tremor worsens by 2% to 5% per year. With the progression of time, there is a tendency for the spread of tremor beyond the arms, such that patients develop cranial tremors (neck, voice, jaw), particularly in women with ET, among whom the risk of neck tremor is severalfold higher than that of men with ET. The prevalence of neck tremor is the highest of these, with voice tremor being less so and jaw tremor being even less so. Neck tremor is generally of a “nono” (i.e., horizontal) variety but can also be a “yes-yes” (i.e., vertical) tremor or a more complex tremor with a rotatory component. Unless severe, the neck tremor, which is a postural tremor, should subside and resolve when the patient is recumbent. Isolated neck tremor, with minimal or no accompanying arm tremor, is extremely rare and should raise suspicion that the diagnosis is dystonia rather than ET. A curious feature of the neck tremor is that patients are often unaware of its presence, particularly when it is mild. The presence of dystonic postures in ET cases is controversial, although it is likely that the presence of mild dystonia in some cases does not preclude a diagnosis of ET, especially when the dystonia is a late finding in a case with long-standing and severe ET.
Although in the past ET was often viewed as a “benign” problem, the term benign essential tremor is no longer considered appropriate. Indeed, the majority of patients have tremor-related disability, and 15% to 25% are sufficiently motorically disabled by high-amplitude shaking that they cannot continue to work.
ET patients have about a fourfold increased risk of developing incident PD, thereby developing what is referred to as essential tremor-Parkinson disease (ET-PD). The pathobiology of this connection is not fully understood.
DIAGNOSIS
Thirty percent to 50% of “ET” cases are misdiagnosed and do not have ET, with many of these cases having dystonia or PD. Differentiation may be made readily, however, by the absence of rigidity or bradykinesia or other signs of parkinsonism (e.g., hypomimia) in these cases. The characteristics of the tremor are also important in distinguishing an ET patient from one with PD (Table 73.1). The presence of isolated postural tremor (with minimal kinetic tremor), a postural tremor involving the metacarpophalangeal joints rather than the wrist, and a postural tremor characterized by greater wrist rotation than flexion and extension are all indicators that the likely diagnosis is emerging PD rather than ET (see Table 73.1). Reemergent tremor is a postural tremor that commences after a brief latency, rather than immediately, and is a feature of PD. Dystonia in the arm is characterized by dystonic posturing (e.g., “spooning of the fingers” [i.e., the tendency during arm extension to flex the wrist and hyperextend the metacarpophalangeal and phalangeal joints]) and the presence of a tremor that is neither rhythmic nor oscillatory. The possibility of neck dystonia should be assessed and is characterized by head tilt or rotation with head tremor,
hypertrophy of the sternocleidomastoid muscle, the presence of a tremor null point, and a sensory trick by history (Table 73.2). Absence of cerebellar speech (i.e., either scanning or dysarthric) and nystagmus distinguishes ET from the spinocerebellar ataxias. Hyperthyroidism or the use of medications such as lithium or valproate is usually excluded by clinical history. A difficult differential is between a mild case of ET and enhanced physiologic tremor, although the presence of neck tremor should exclude the latter. Computerized tremor analysis, with inertial loading, can assist with this differential. In patients with a tremor of central origin (ET), the primary tremor frequency should not change with inertial loading.
hypertrophy of the sternocleidomastoid muscle, the presence of a tremor null point, and a sensory trick by history (Table 73.2). Absence of cerebellar speech (i.e., either scanning or dysarthric) and nystagmus distinguishes ET from the spinocerebellar ataxias. Hyperthyroidism or the use of medications such as lithium or valproate is usually excluded by clinical history. A difficult differential is between a mild case of ET and enhanced physiologic tremor, although the presence of neck tremor should exclude the latter. Computerized tremor analysis, with inertial loading, can assist with this differential. In patients with a tremor of central origin (ET), the primary tremor frequency should not change with inertial loading.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree