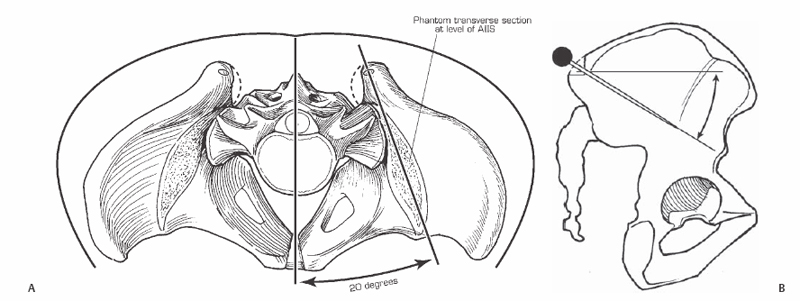
40 James S. Harrop, Shiveindra Jeyamohan, and Alexander R. Vaccaro Intra-iliac screw placement entails a pelvic screw anchor used to fixate the lumbosacral spine to the pelvis for stability and deformity correction in long or multisegmental fusions, high-grade spondylolisthesis, of pelvic obliquity deformity correction. Posterior intra-iliac fixation provides a biomechanical advantage over sacral instrumentation through secure anchors in the pelvis. The screws cross anterior to the sagittal vertical axis or sagittal plumb line without violating the sacroiliac joints. Intra-iliac fixation provides a solid distal foundation (pelvis) for the correction of spinal deformities, long spinal constructs, or high-grade spondylolisthesis. Need for plain radiographs of the thoracolumbar spine including standing long cassette views (36-inch) to evaluate coronal and sagittal balance. Plain radiographs of the pelvis as well as dynamic lateral flexion and extension images of the lumbar spine. In revision cases, particularly ones where there was prior posterior iliac crest bone graft harvest, a computed tomography (CT) scan of the pelvis provides further information. Placement of the iliac screw from the contralateral side of the table provides for a more optimal sense of screw trajectory. An osteotomy or harvesting bone from the posterior iliac crest can result in weakening of the insertion site. Therefore, bone graft harvesting should be planned after iliac screw placement. Intraoperative fluoroscopy or plain radiographs can evaluate the final position of screw placement: Placement of S1 screws should be done prior to iliac screws placement. This provides for an accurate assessment of screw-to-screw distance and optimal iliac screw to facilitate construct assembly. Surgical exposure is performed with a posterior midline incision down to the spinous processes of the lumbosacral junction. The posterior superior iliac crest can be palpated and the erector spinae muscles are dissected from the midline in a medial to lateral direction in a subperiosteal manner to the medial border of the iliac crest, taking care not to disrupt its distal insertion to maintain muscle viability and prevent the formation of a dead space. The soft tissues (gluteal muscle attachments) on the lateral iliac crest wall are dissected off the ilium in a subperiosteal manner to allow finger palpation of the sciatic notch. The starting point for iliac screw placement is often the distal prominence of the posterior superior iliac crest, which is anatomically located directly lateral to the S2 pedicle (Fig. 40.1 and 40.2). Precise screw starting point, however, is guided by the location of the sciatic notch, which is felt during screw path development.
Intra-Iliac Screw/Bolt Fixation
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







