(MFV, SPR)
(MFV, SPR)
(MFV, SPR)
ACA: anterior cerebral artery; BA: basilar artery; MCA: middle cerebral artery; MFV: mean flow velocity; n.a., not available; PCA: posterior cerebral artery; SPR: stenotic/prestenotic MFV ratio; VA: vertebral artery.
| Artery | Mild stenosis | Moderate stenosis | Severe stenosis |
|---|---|---|---|
| Stenosis ≤50% (PSV) | Stenosis ≥50% (PSV) | Stenosis >80% | |
| MCA | ≥155 cm/s | ≥220 cm/s | + Indirect signs |
| ACA | ≥120 cm/s | ≥155 cm/s | + Indirect signs |
| PCA | ≥100 cm/s | ≥145 cm/s | + Indirect signs |
| BA | ≥100 cm/s | ≥140 cm/s | + Indirect signs |
| VA | ≥90 cm/s | ≥120 cm/s | + Indirect signs |
ACA: anterior cerebral artery; BA: basilar artery; MCA: middle cerebral artery; PCA: posterior cerebral artery; PSV: peak systolic velocity; VA: vertebral artery.
Indirect signs: proximal and/or distal flow alterations (i.e., diastolic velocity drop and high resistance in the feeding vessel or in the proximal segment of the stenotic vessel, a delayed systolic flow rise and velocity drop downstream, flow diversion and signs of collateralization).
However, none of these criteria are absolute, consequently it is important to validate these velocity values in each neurosonological laboratory against angiographic findings.
For a more systematic approach, we recommend following these direct criteria: the first criterion for intracranial stenosis, applicable only to TCCS, is represented by a color aliasing phenomenon, which may indicate the presence of raised flow velocities, such as those caused by a stenosis, and will help guide spectral Doppler interrogation [12] (Figure 10.1); note that a turbulent flow is also a frequent physiological finding caused by a tortuous vessel course.
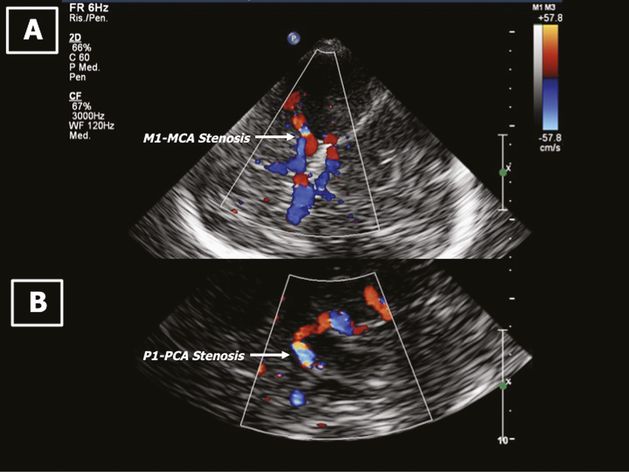
Color aliasing phenomenon indicates the presence of a stenosis. (A) M1 segment of the MCA; (B) P1 segment of the PCA.
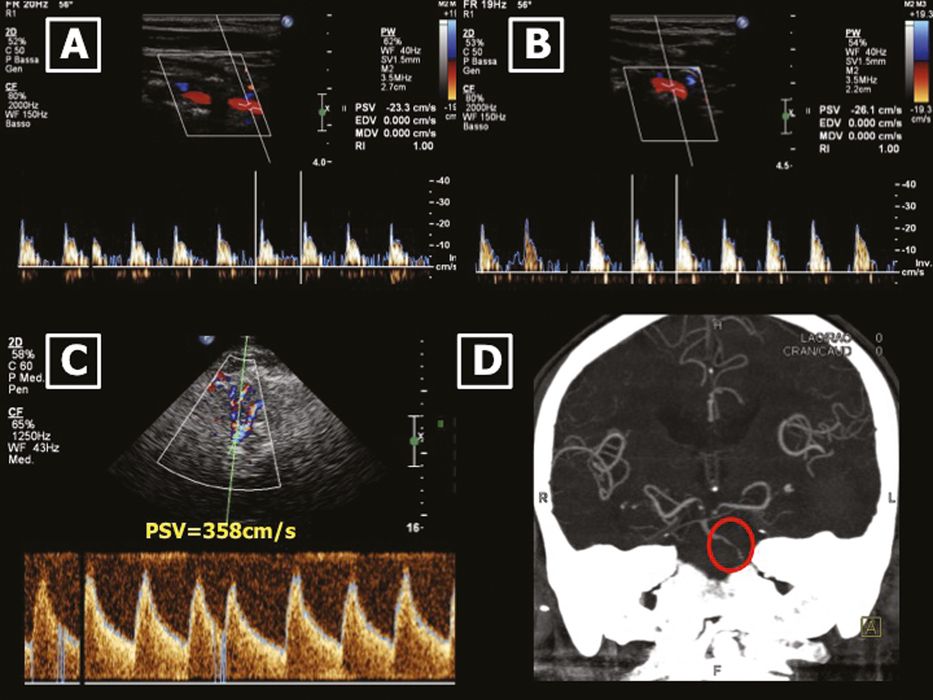
The second criterion is a progressive focal increase of blood flow velocities in ≥50% stenosis (Figure 10.2) or paradoxical velocity decrease with very severe stenosis, near-occlusion or diffuse intracranial disease. As a rule for a vessel with straight walls, a 50% diameter reduction doubles the velocity, and a 70% stenosis may triple the velocity at the end of the stenosis compared with a prestenotic segment or with the contralateral nonaffected side [13].
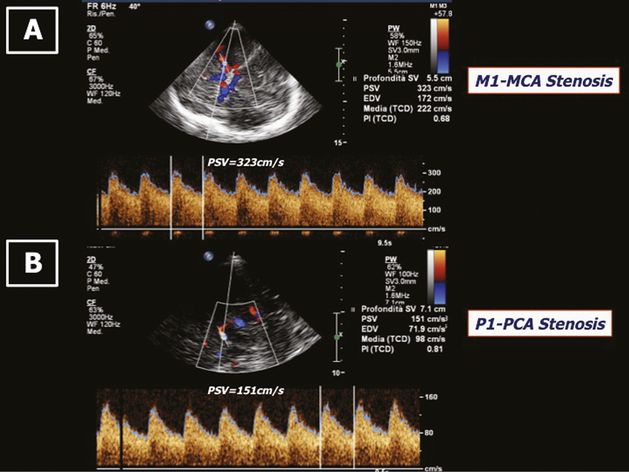
A focal increase of blood flow velocities indicating a hemodynamic significant stenosis. (A) M1 segment of the MCA; (B) P1 segment of the PCA.
It is noteworthy that the velocity values measured by TCCS are higher than those by TCD if there is angle correction. Angle correction should be performed when the Doppler sample volume is located within a straight vessel segment ≥20 mm in length [14]. In contrast with the extracranial internal carotid artery, intracranial arteries do not have a bulbous widening at their origin; this means that flow velocity changes are already observed with a diameter reduction <50%, hence even a 30–50% stenosis will result in a detectable flow velocity increase. On the contrary, in certain vessels segments of the intracranial circulation (e.g., P1-PCA, A1-ACA) there might be no significant flow velocity increase, despite the presence of a stenosis, due to efficient collateralization (via ipsilateral internal carotid artery and posterior communicating artery – PCoA, and via contralateral A1 and anterior communicating artery – ACoA, respectively).
A third diagnostic criterion for intracranial stenosis is a significant (≥30%) side-to-side difference of velocity; however, this criterion can only be applied to symmetrical vessel segments after accurate angle correction. In the case of severe stenosis, two additional frequent findings are co-vibrations (i.e., high-intensity signals at the zero line) and musical murmurs, which have a visual correlate called mirror-image parallel strings (Figure 10.3).
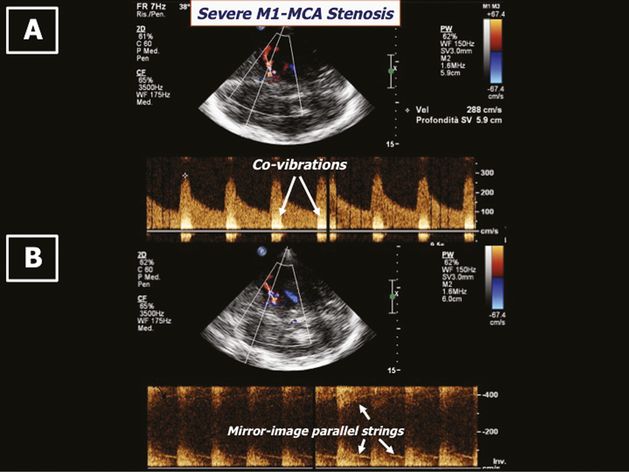
Signs of a severe stenosis of the M1 segment of the MCA. (A) Co-vibrations; (B) mirror-image parallel strings.
Musical murmurs, in very high-grade stenosis, are harmonic phenomena resulting from harmonic frequencies generated from regular vibrations of the vessel walls caused by the increased flow velocities and sound like a musical tone (sea gull cry, goose cry, honks, cooing). Beware that murmurs are also found in functional stenoses when blood flow is too high for the size of the vessel (ACoA, PCoA).
In very severe stenosis (>80%), in addition to the direct criteria described previously, there are indirect hemodynamic criteria which include proximal or distal flow alterations: a diastolic velocity drop and high resistance in the feeding vessel or in the proximal segment of the stenotic vessel, a delayed systolic flow rise and velocity drop (tardus et parvus) downstream, flow diversion and signs of collateralization (Figures 10.4 and 10.5).
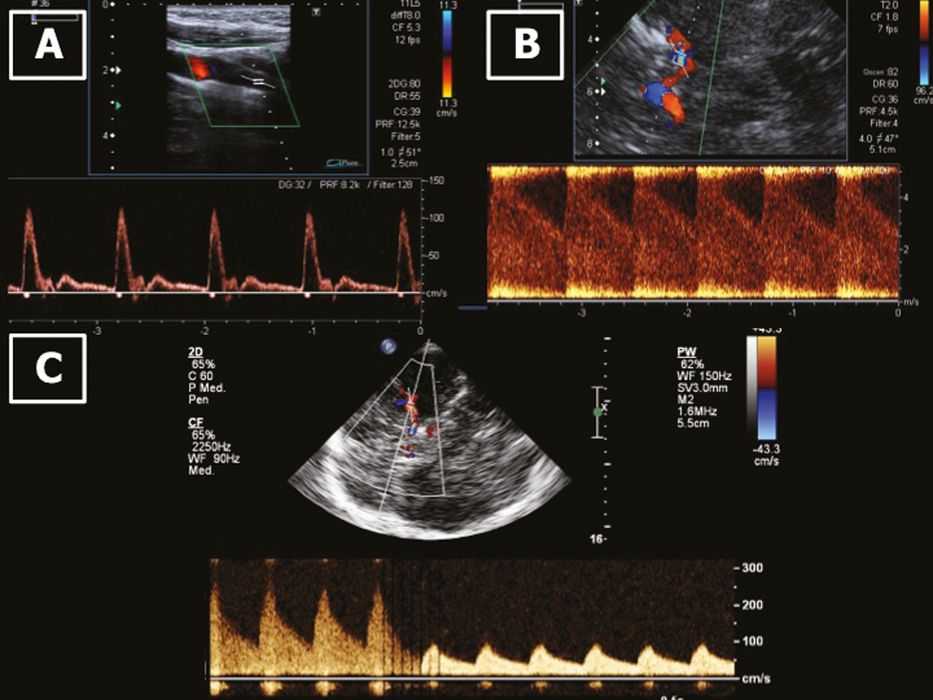
Indirect hemodynamic signs. (A) Prestenotic diastolic drop (with retained diastolic component) and increased peripheral resistance in the ipsilateral ICA of a patient with (B) a severe MCA stenosis. (C) Poststenotic delayed systolic flow rise and velocity drop in a patient with a severe MCA stenosis.
Indirect hemodynamic signs. (A) and (B) prestenotic diastolic drop and increased peripheral resistance in both vertebral arteries. (C) A significant focal increase of blood flow velocities, and (D) angio-CT image indicating a severe basilar artery stenosis.
When the bone window is inadequate or absent, ultrasound contrast agents should be used in order not to miss hemodynamically significant stenoses (Figure 10.6).
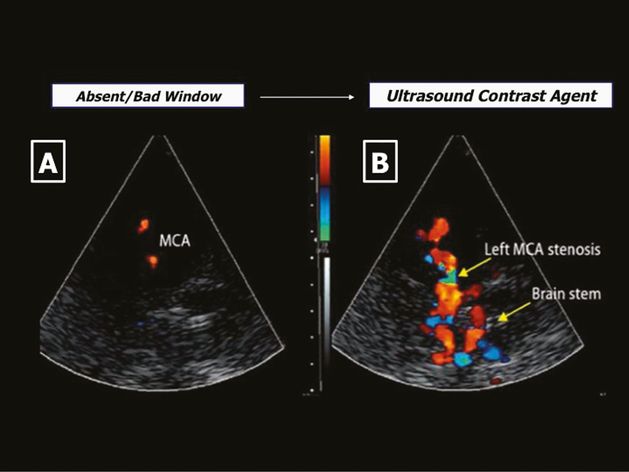
(A) Inadequate transtemporal bone window; (B) ultrasound contrast agent disclosing a >50% MCA stenosis.
Analogously, if a high-grade intracranial vertebral artery or basilar artery stenosis must be quickly ruled out, contrast agents should be used generously for an accurate diagnosis, being aware that prestenotic flow in patients with distal basilar artery stenosis may be normal.
Occlusion
Direct criteria for proximal occlusion include the complete absence of color-flow signal (using lowest pulse repetition frequency [PRF] and increased color-gain settings) (Figure 10.7) or minimal flow signal in vessel segments (branches or perforators) proximal to the occlusion; criteria for distal occlusion are blunted flow signal and dampened flow signal as discussed in greater detail in Chapter 12, since most evaluations concerning intracranial occlusions are made in acute stroke patients.
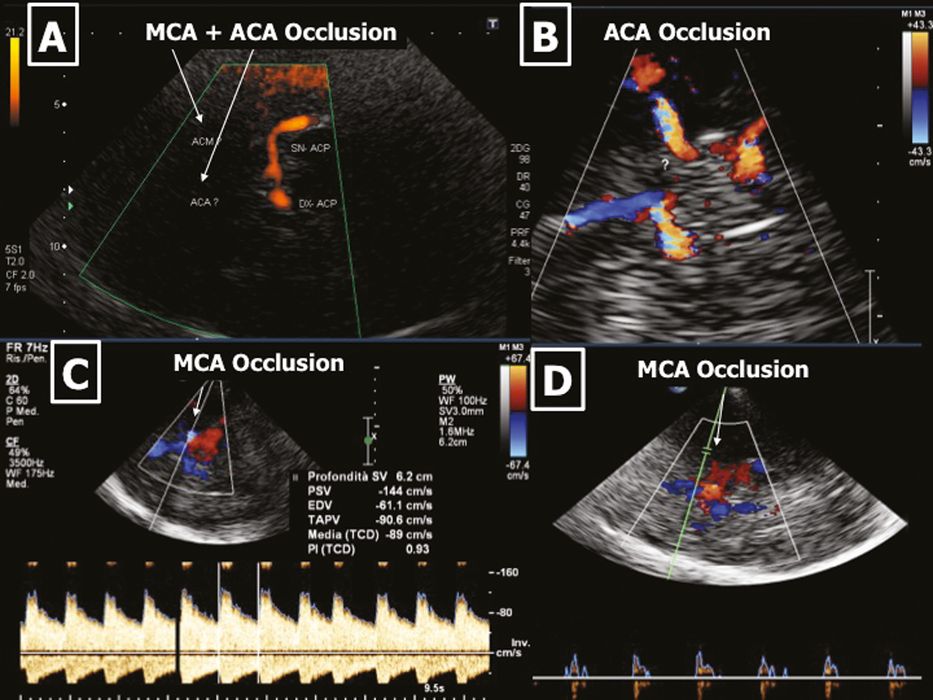
Intracranial artery occlusion. (A) Absent signal in the MCA and ACA, while it is present in the PCA. (B) Absent color Doppler signal in ACA even after ultrasound contrast agent administration. (C) No color signal in the MCA, flow diversion in the ACA. (D) No color and Doppler signal in the MCA.
It is noteworthy that a missing flow signal does not necessarily imply occlusion – it could be hypoplasia/aplasia. It is therefore helpful to use ultrasound contrast agents and very important to check for indirect signs of intracranial occlusion in the proximal and distal vessel segments: a diastolic velocity drop and high resistance in the feeding vessel or in the proximal segment of the occluded vessel; a flow diversion; a post-occlusive orthograde flow pattern if efficient collaterals distal to the occlusion are activated; sometimes a flow inversion is observed distally (Figure 10.8). For example, in a proximal basilar artery occlusion, activation of the PCoAs with retrograde flow in the posterior cerebral arteries and in the distal segment of the basilar artery is a frequent finding, along with a positive oscillation phenomenon with carotid tapping. Beware that there are no indirect signs in patients with top of the basilar artery occlusion, so that an apparent normal flow in the vertebral arteries and in the proximal basilar artery does not exclude distal basilar artery occlusion. A helpful trick in this case is to tap the vertebral arteries: if this determines an oscillation of the flow in the posterior cerebral arteries, then a complete basilar artery occlusion can be excluded.
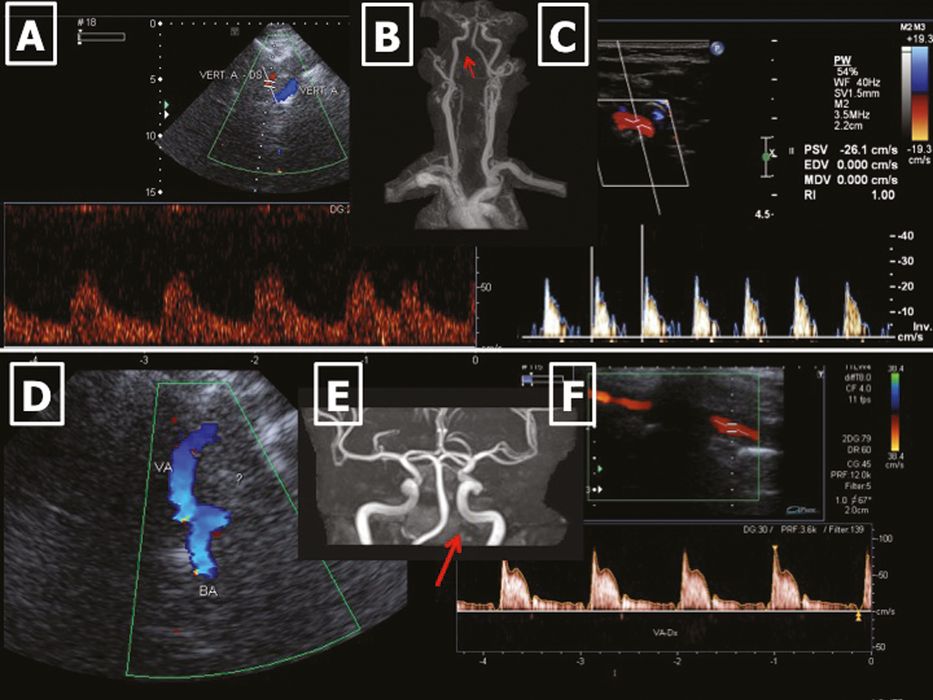
(A–C) Pre-posterior inferior cerebellar artery (PICA) occlusion of the intracranial segment – V4 – of the vertebral artery. (A) Flow inversion in the V4 segment distally to a pre-PICA occlusion. (B) Missing V4 segment (red arrow) in magnetic resonance angiogram (MRA). (C) Prestenotic very high resistance flow in the ipsilateral V2 segment (note that the diastolic component is missing). (D–F) Post-PICA occlusion of the intracranial segment – V4 – of the vertebral artery. (D) No color signal in the V4 segment. (E) Missing V4 segment (red arrow) in MRA. (F) Prestenotic high resistance flow in the ipsilateral V2 segment (note that the diastolic velocity component is reduced but present).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








