Fig. 16.1
Clear cell (lipid-rich) variant of pancreatic neuroendocrine tumor in (a). Oncocytic variant of pancreatic nonfunctioning neuroendocrine tumor in (b)
Among prognostically relevant histologic findings, there are vascular invasion (Fig. 16.2), perineural invasion, focal necrosis, mitotic index, and the percentage of cells reactive for proliferative markers like Ki67 protein [8, 15–17]. In general no difference has been found in nonfunctioning compared to functioning neoplasms, with the Ki67 index proving more sensitive and effective than the mitotic index to grade neuroendocrine neoplasms as grade 1 or 2.
Fig. 16.2
Nonfunctioning pancreatic neuroendocrine tumor, grade 2 (WHO 2010), showing angioinvasion (a, high magnification in b). This tumor is immunoreactive for chromogranin A (c) and exhibits a Ki67 proliferative index of 20 % (d). The mitotic index is 10 mitoses/10 HPFs. The differential diagnosis with a neuroendocrine carcinoma (NEC) is challenging
Of special interest is the histologic evaluation of incidentally found neoplasms, most of which proved to be grade 1, in the absence of microvascular or perineural invasion and of macroscopic signs of invasion or metastasis [6]. Indeed, incidental grade 1 cases (with 0–2 % of Ki67 index and a mitotic index less than 2/10 HPFs, high-power fields) less than 2 cm in size seem to be appropriate candidates for studies concerning conservative managements of pancreatic neuroendocrine neoplasms, especially in patients at increased surgical risk due to coexisting morbidities.
Immunohistochemical tests showed a variety of hormones in nonfunctioning neoplasms, including pancreatic polypeptide (PP), glucagon, somatostatin, insulin, serotonin, calcitonin, gastrin, vasoactive intestinal peptide (VIP), ghrelin, neurotensin, and ACTH in a roughly decreasing order of frequency [8, 18]. They often coexisted in the same “multihormonal” tumor as minor or major cell populations, together with a variable (often large and overwhelming) proportion of hormone-unreactive cells.
It appears that neoplasms producing PP, glucagon, and somatostatin have a higher tendency to remain nonfunctioning, even when showing high hormone contents, compared to neoplasms producing powerful hormones like insulin, gastrin, or VIP, affecting clinically more relevant functions. Consequently, in multihormone-producing neoplasms, the predominant hormone produced or tumor cell type expressed is not necessarily the one accounting for the associated hyperfunctional syndrome. This has been repeatedly observed for predominantly PP cell neoplasms, whose associated watery diarrhea, hypokalemia, and achlorhydria (WDHA) or Zollinger-Ellison (ZE) syndromes were often found to be accounted for the minority populations of VIP-producing cells or gastrin-producing cells, respectively [19–23]. Similar findings have been obtained for neurotensin-producing tumors in respect to WDHA or ZE syndromes [24–26].
Given their large proportion of hormonally unreactive cells and/or the limited clinical impact of the hormones they actually produce, the diagnosis of nonfunctioning neoplasms should be based chiefly on their reactivity toward general neuroendocrine markers like chromogranin A, synaptophysin, neuron-specific enolase, or PGP 9.5 (i.e., ubiquitin hydrolase L1), more than on the individual hormones produced.
Besides being observed in neoplastic cells, pancreatic polypeptide has been frequently found to be increased in serum of patients bearing neuroendocrine neoplasms, though in the absence of any sign of pertinent hyperfunction [23, 24]. Based on these findings, serum PP level measurements have been proposed as a useful test to detect occult pancreatic neuroendocrine neoplasms. Although it has been suggested that the majority of neoplasms purely or predominantly composed of PP cells (Fig. 16.3) have a benign behavior, it should be outlined that several malignant cases causing patient death have been also reported [18, 20–23].
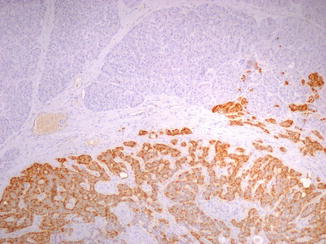
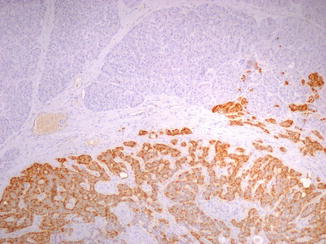
Fig. 16.3
PP-producing pancreatic neuroendocrine tumor (microadenoma) in a MEN1 patient: PP immunostain shows a diffuse and strong positivity
Calcitonin-producing pancreatic neoplasms are quite rare. A search in 2011 identified 37 cases, many of which, in addition to calcitonin, also produced multiple other hormones, among which somatostatin, VIP, PP, insulin, gastrin, and glucagon, like most other nonfunctioning neoplasms [27]. However, a frequent (19/37 cases) association with watery diarrhea (WDHA) syndrome was noted, in several cases coupled with, and likely due to, increased blood levels of VIP produced by tumor tissue. In other cases, no VIP increase in serum was detected and a possible role of calcitonin itself was proposed, also considering the frequent association of the watery diarrhea syndrome with calcitonin-producing thyroid medullary carcinoma, with or without associated VIP production. The rare pancreatic metastases from thyroid medullary carcinoma should be considered in the differential diagnosis [28]. Most (60 %) calcitonin-secreting pancreatic neoplasms proved metastatic [27], a finding confirming previous suggestions on histochemical grounds that calcitonin expression by tumor cells may represent an unfavorable prognostic sign [8].
16.3 Diagnosis
The distinction between functioning and nonfunctioning pancreatic neuroendocrine tumors is made solely on the basis of the clinical picture, as nonfunctioning pancreatic neuroendocrine tumors are not associated with a distinct clinical syndrome. However, they may produce hormones that can be detected as abnormally increased serum levels or by immunohistochemical stainings on tumor tissue. Incidentally discovered nonfunctioning tumors have been increasingly detected in recent years due to high-resolution imaging techniques [5] and should be separated from those presenting with symptoms of an expanding mass in the upper abdomen or of tumor infiltration of neighboring organs.
16.4 Prognosis
In nonfunctioning pancreatic neuroendocrine neoplasm, the most important factors predictive of aggressive behavior include grade and stage. As a rule, production of specific peptides has no major impact on survival. Recent data from 1,072 patients who underwent surgery for neuroendocrine neoplasms of the pancreas suggest that the European Neuroendocrine Tumor Society (ENETS) TNM staging system is superior to the International Union for Cancer Control/American Joint Cancer Committee/World Health Organization (UICC/AJCC/WHO 2010) TNM staging system and, for nonfunctioning tumors, reported a death rate per 100 person-years of 4.5 [17].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







