INTRODUCTION
Parkinson’s disease (PD) is prevalent worldwide, and the number of occurrences is predicted to rise (1) and is ranked as the second commonest neurodegenerative disorder (2). Traditionally, PD is typically characterized by its motor symptoms, namely rigidity, resting tremor, bradykinesia, and postural instability. However, this concept has changed mainly in the 21st century and PD is now regarded as much a nonmotor disorder as a motor disorder. The range and burden of nonmotor symptoms (NMSs) reflect a key determinant of the patient as well as carer’s quality of life and possibly, presents the biggest challenge to clinicians and health-care professionals dealing with PD (3,4). In addition, several studies have shown the serious social and economic consequences related to NMS which frequently cause hospitalization and institutionalization (5,6). Nevertheless, for many, NMSs remain widely regarded as peripheral, which leads to a suboptimal clinical care and quality of life of patients as well as carers (7). Regardless of the duration of the disease and the motor stage, a typical patient with PD experiences an average of 8 to 13 NMSs (8) even at a very early and untreated stage of the condition.
Why is PD a nonmotor disorder as much as a motor disorder? The evidence for this is multifactorial. Some key issues supporting the notion that PD is as much a nonmotor than a motor disorder are provided in the following (9):
• Historical:
• James Parkinson outlined several nonmotor issues such as sleepiness, cognitive problems, and autonomic dysfunction in his original essay describing PD. This was then reflected in description of PD symptoms by others such as Gowers (10).
• Frederick Lewy described Lewy bodies in the dorsal motor vagal nucleus in 1913.
• Some have considered PD to be a neurospychiatric disorder.
• NMS as premotor feature: Some NMSs can predate motor symptoms by up to 10 to 15 years (such as late-onset idiopathic hyposmia and rapid eye movement [REM] sleep behavior disorder) (11).
• The burden of NMS:
• The burden of NMS (as opposed to individual NMS) appears to be the key determinant of quality of life of people with Parkinson’s (7).
• The burden of NMS can be severe even in untreated PD, contrary to common perception (12).
• Patient rating:
• Patients consistently rate NMS as most bothersome using validated self-declarations tools such as the NMSQuest (13).
• Specific patterns of NMS complicate early-onset versus late-onset PD.
• Pathology:
• Pathology of PD includes degeneration of nondopaminergic nuclei and pathways, including serotonergic, cholinergic, and noradrenergic, from the onset of illness and sometimes differentially more affected than dopaminergic nuclei.
• Differential Lewy body deposition sites in the brain in early-onset versus late-onset PD (14).
PATHOPHYSIOLOGY
It is now acknowledged that PD is a progressive multiorgan disease due to deficits in multiple neurotransmitter pathways, including the cholinergic, noradrenergic, and serotonergic systems (14–16) and not a single neurotransmitter (dopaminergic)-mediated disorder. Evidence suggests that the condition may have central nervous system as well as extra-central nervous system origins, notably in the enteric nervous system (17). Multiple dopaminergic and nondopaminergic dysfunctions lead to the presentation of numerous NMSs such as depression, anxiety, sleep disorders, autonomic dysfunction, and cognitive dysfunction. The degenerative process of nondopaminergic neurones may start well before the presentation of motor symptoms (Table 6.1).
In 1913, Lewy bodies in the dorsal motor vagal nucleus were described by Frederick Lewy, suggesting a nondopaminergic onset of PD if one considers that Lewy body deposition is consistent with neuronal degeneration. In the 1920s, Braak proposed a six-stage pathologic process based on Lewy body formation with a “bottom up” theory of pathogenesis of PD veering away from the traditional concept that PD starts with degeneration of the substantia nigra neurones. He suggested that stage one begins with the degeneration of the olfactory bulb and the anterior olfactory nucleus and the lower medulla, while stage two reflects the pathologic process affecting the lower brain stem with involvement of serotonin (median raphe) and noradrenaline (locus coeruleus) nuclei in the brain stem and pons (25,26). Clinically, this progression results in a range of NMSs such as late-onset hyposmia (olfactory bulb and nucleus) as well as REM behavior disorder (RBD) (lower brain stem) both symptoms being recognized as premotor markers of PD (see Table 6.1). In addition, some key NMS such as olfaction, sleep homeostasis, depression and cognition, pain, constipation, and central autonomic vagal control are mediated by lower brain stem nuclei. Progression to stages three to six of Braak is thought to correlate with motor stages of PD and development of further NMS such as cognitive dysfunction and autonomic dysfunction common in the advanced stages of PD.
| Nondopaminergic Involvement in PD at a Premotor and Early Motor Stage |
Author, year | Evidence of Nondopaminergic Involvement in PD at a Premotor and Early Motor Stage |
Forno, 1996 (18) | Lewy bodies were first reported in nondopaminergic neurones. |
Jellinger, 1987 (19) Halliday, 1990 (20) | Cholinergic pedunculopontine nucleus neurones and substance P–containing neurones suffer 77% loss in dorsal motor nucleus of the vagus, while tyrosine hydroxylase–immunoreactive neurones appear spared (<5%) |
Hirsch, 1987 (21) | Neuronal loss in dorsal motor nucleus of the vagus is as marked as in the substantia nigra. |
Saper, 1991 (22) | Complete sparing of medullary dopaminergic neurones described |
Wakabayashi, 1997 (23) | Lewy body degeneration is prominent in the nondopaminergic anterior olfactory nucleus. |
| Noncatecholaminergic neurones severely depleted in PD in the autonomic system: spinal intermediolateral nucleus 30%–40% loss of preganglionic autonomic neurones |
| Lewy bodies are frequent in the vasoactive intestinal peptide neurones of the enteric nervous system but rare in catecholaminergic cells. |
Lewy bodies present in both TH+ and TH− cells in the cardiac plexus. | |
Braak, 2003 (25) | Lewy body degeneration developing in lower brain stem neurones well before the substantia nigra. |
Braak, 2004 (26) | Incidental Lewy bodies identified within pontomedullary neurones in the absence of substantia nigra pathology, but not vice versa |
PD: Parkinson’s disease; LB: Lewy bodies; TH: tyrosine hydroxylase Source: Adapted from Todorova A, Jenner P, Ray Chaudhuri K. Non-motor Parkinson’s: integral to motor Parkinson’s, yet often neglected. Pract Neurol 2014;14:310–322. | |
THE PROBLEM OF ANIMAL MODELS FOR NMS IN PD: AN UNMET NEED
Since 2000, the clinical phenomenology of NMSs of PD and the development of validated rating scales have made major advances, which has led to better understanding of the evolution and progression of NMS. However, the use of experimental models to assist in understanding pathogenesis and potential approaches to treatment has remained a key unmet need and while opportunities offered by existing dopaminergic animal models (which may be inadequate considering the multi-neurotransmitter deficiencies seen in PD) are being refined, models for the investigation of dopamine dysregulation syndromes/compulsive behaviors and dopamine agonist withdrawal syndromes (DAWS) are yet to be developed. Development of an animal model that shows the overall pathology of PD and its progression is thus important and continue to be an unmet need. A list of animal models addressing NMS are listed in Table 6.2.
WHAT ARE THE NMSS THAT OCCUR IN PD?
Besides the description of the motor impairment, James Parkinson already mentioned sleep disturbance, constipation, dysarthria, dysphonia, dysphagia, urinary incontinence, and “at the last, constant sleepiness with slight delirium” (31), all referring to the burden of NMS (32). Indeed, NMSs include symptoms such as autonomic, psychiatric, sleep, and pain which demonstrate the wide range of neuropeptide involvement affecting the central and peripheral nervous system. Furthermore, NMS in PD may be due to drug therapy or disease-related complications. While some NMSs are present in the “premotor” stage (impaired olfaction and autonomic dysfunction, depression), some dominate in the early and untreated phase of PD, while others seem to affect the clinical picture throughout (pain, fatigue) and particularly PD at its later advanced stages (dementia, apathy, dysautonomia) (33–35). Todorova et al. (36) have attempted a classification in order to further categorize the causes of the wide variety of different NMSs in PD recognizing that NMS can be disease related to therapy of PD:
| A List of Proposed Parkinsonian Animal Models Addressing Nonmotor Symptoms and Exploration of Pathophysiology |
Animal Model | Nonmotor Symptoms |
6-OHDA–lesioned rodents (27) | Olfaction Sensory/pain threshold Sleep/wakefulness Circadian rhythms Cognitive function (Altered cardiovascular function) (Bladder hyperactivity) (Altered motility of gastrointestinal tract) |
α-Synuclein overexpressor (ASO = Thy1-aSYN) mice (28) | Olfaction Autonomic Constipation Sleep Cognition |
MPTP-treated primates (27) | Bladder hyperreflexia Constipation Drooling Altered cardiovascular function Sleep disturbance Cognitive disturbance |
Mice model of intragastric rotenone administration (29) | α-Synuclein accumulation in dorsal vagal nucleus Potential for investigating autonomic symptoms such as constipation |
Göttingen minipigs (Ellegaard Minipigs ApS) (30) | Cognition/sleep |
OHDA, hydroxydopamine; MPTP, 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine. Source: Adapted from Todorova A, Jenner P, Ray Chaudhuri K. Non-motor Parkinson’s: integral to motor Parkinson’s, yet often neglected. Pract Neurol 2014;14:310–322. | |
• Related to the disease process or pathophysiology
• Dopaminergic origin/Nondopaminergic origin
• Related to a partial nonmotor origin (usually brain stem autonomic impairment with motor end result, such as constipation or diplopia)
• Related to nonmotor fluctuations (NMFs) (cognitive, autonomic, and sensory subtypes)
• Could be fluctuating NMS
• Or only present at off period
• Related to PD drug therapy
• Specific symptoms (such as hallucinations, delirium)/Syndromes (impulse control disorders [ICDs], DAWS, Parkinson’s hyperpyrexia syndrome (thermoregulatory failure, delirium)
• Possibly genetically determined
• Higher risk of dementia in cases or carriers with glucocerebrosidase mutation
• Higher risk of depression and sleep disorders in cases with leucine-rich repeat kinase-2 mutation
Prevalence studies in NMS, using a holistic approach, have only been possible till the validation of holistic NMS tools such as nonmotor symptoms scale (NMSS) or nonmotor symptoms questionnaire (NMSQuest) in 2006/2007. Several studies have since emerged addressing NMS prevalence in over 2,500 patients across the world in different clinical setup as well as population base. Three studies have compared NMSQuest scores in a controlled manner, and data suggest that irrespective of the motor stage of PD, a typical patient will present with at least 8 (range 4–19) different NMSs compared to a health-control subject who would present 3 to 4 NMSs (4–12).
In a study by Politis et al (13), the authors reported that symptoms such as pain, sleep disorders, and anxiety are rated by patients with early (within 6 years) and advanced PD as “most bothersome” ahead of motor symptoms (13,37). As a consequence, these NMSs have a key impact of the patient’s quality of life, which has been reported in a large (over 8,000 patients included) NMSQuest-based study (38). Other European studies such as the PRIAMO study have demonstrated that NMSs have the closest correlation with health-related quality of life (HRQoL) (39). PRIAMO and other large-scale studies have shown that patients with the highest NMS scores had the worst HRQoL (7,39,40).
PREMOTOR NMS IN PD
Currently, PD is still diagnosed using the UK PD Brain Bank criteria being completely based on motor symptoms, excluding key NMS such as hyposmia in the criteria and even listing autonomic dysfunction as an exclusion criteria (41,42). This fact has provoked researchers and clinicians to redefine PD and the diagnostic criteria. Recent view is that PD could be subdivided into a preclinical (could be detected in future by biomarkers such as imaging or genetic screening), premotor, and motor stage, with NMS being the dominant “marker” of the premotor stage (4,11). Studies such as the “Parkinson’s at risk syndrome” study have suggested that it is possible to identify certain NMSs that can help as premotor markers of PD to predict the onset and prognosis of the disease (Table 6.3). Late-onset and idiopathic hyposmia as well as RBD seem to be robust premotor markers (53,54), and studies have reported that patients demonstrating “idiopathic” RBD have a 25% to 40% risk to develop a synucleinopathy such as PD in 5 years’ time and a 40% to 65% risk in 10 years’ time (44). Similarly, Jennings et al. (43) have reported evidence that a high rate of patient suffering from “idiopathic” hyposmia who also show reduced dopamine transporter activity will further develop motor PD. A recent review concludes that the identification of people with constipation/postural instability, mild memory disorder, depression/anxiety, visual hallucinations/psychosis (particularly in older patients), and RBD associated with a decreased uptake of MIBG might help to detect patients with Parkinson’s before the actual onset of motor symptoms such as tremor, bradykinesia, and rigidity (55). Recently, Sixel-Doring et al. (45) have described novel REM sleep behavioral events (RBE), which tend to occur more frequently in patients with de novo PD compared to healthy controls and thus could be considered as an early sign of neurodegeneration which precedes REM sleep behavior disorder.
| Currently Reported Premotor Nonmotor Symptoms Which Could Potentially Emerge as Biomarkers for Premotor PD |
Nonmotor Symptoms | Relevant Findings Reported |
Late-onset hyposmia | Hyposmia and abnormal DATScan may suggest 43% develop motor PD in 4 years (43). |
Rapid eye movement sleep behavior disorder | 25%–40% risk to develop PD at 5 years, 40%–60% at 10 years (44) |
Rapid eye movement behavior events | First study reported 2014 (45) |
Constipation | 2.7–4.5 times excess in the risk of PD in men with <1 bowel movement/day (46) |
Major depression | Increased risk to develop PD (47) |
Excessive daytime sleepiness | Three times excess in the risk to develop PD (48) |
Erectile dysfunction | 3.8 times more likely to develop Parkinson´s disease (49) |
Pain | Increased risk to develop PD (50) |
Fatigue | Increased risk to develop PD (51) |
Visual impairment (contrast sensitivity, color vision, etc.) | Case studies (52) |
Source: Adapted from Sauerbier A, Ray Chaudhuri K. Non-motor symptoms: the core of multi-morbid Parkinson’s disease. Br J Hosp Med (Lond) 2014;75:18–24. | |
NONMOTOR FLUCTUATIONS
Whereas motor fluctuations are extensively described during on and off periods in PD, fluctuations in relation to the NMS have been less studied. It might be possible to divide the NMFs in two different categories (56). While some NMSs are also present during “on” periods and worsen during motor “off” periods, others specifically only present during “off” periods (56). This association has important consequences for the management of NMS as in those with purely “off”-related NMS such as depression; the treatment needs address of off-period abolition and not use of antidepressants. Another important aspect of NMF is early morning off (EMO) states which could be associated with a range of NMS. A large European study reported an overall prevalence of 59.7% EMO in a consecutive cohort of 320 treated PD patients of which 88% reported NMS specific to EMO some of which had never been discussed with the physicians (57).
DRUG-RELATED NMS
A range of NMS occurs due to treatment-related causes and are listed in the classification of NMS (Table 6.4). In clinical practice, this is largely reflected in the neuropsychiatric side effects and behavioral problems (ICDs and dopamine dysregulation syndromes) related to dopaminergic therapies, a withdrawal syndrome similar to substance abuse withdrawal (DAWS) and rarely drug interaction (autonomic symptoms of serotonin syndrome, for example). A study by Kim et al. (58), including de novo PD patients, has shown that excessive daytime sleepiness, restless leg syndrome, attention deficit, urinary symptoms, and hyposmia, are useful markers of the disease-related process and can be helpful in differentiating between dopaminergic and nondopaminergic NMSs. Specifically, ICD, including behaviors such as pathologic gambling, compulsive buying, compulsive sexual behaviors, and binge or compulsive eating (59), presents a major challenge to the management of PD. Estimated prevalence of ICD is 14% to 17% with dopamine agonists (DAs) therapies, although there is overlap with levodopa therapy (punding, for example) and dopamine dysregulation syndrome appears related to levodopa intake. Some argue that these rates are underestimated (60), and an additional challenge is that sudden stoppage of DAs can lead to the DAWS (61). DAWS cause a wide range of symptoms such as panic attacks, anxiety, social phobia, depression, vomiting, and symptomatic orthostatic hypotension (61) (62) and do not respond to levodopa, antidepressants, and anxiolytics but may improve with cautious reintroduction with low-dose DA (61).
| A List of NMS That May Be Precipitated by Dopaminergic Treatment in PD |
Autonomic | Parkinson hyperpyrexia syndrome or neuroleptic malignant syndrome* Serotonin syndrome† Malignant parkinsonism* Orthostatic hypotension |
Fibrotic complications | Cardiac Retroperitoneal Pleuropulmonary |
Behavioral/Neuropsychiatric | Hallucinations Delusions Delirium Dopamine dysregulation syndrome Punding Impulse control disorders (ICDs) Dopamine agonist withdrawal syndrome (DAWS)* |
Sleep related | Excessive daytime sleepiness |
Gastrointestinal | Nausea Diarrhea (usually related to intake of COMT inhibitors) |
*On dopaminergic drug withdrawal. †Interaction of MAO-B inhibitors and tricyclic antidepressants and selective serotonin-reuptake inhibitors frequently implicated. Source: Adapted from Chaudhuri KR, Schapira AH. Non-motor symptoms of Parkinson’s disease: dopaminergic pathophysiology and treatment. Lancet Neurol 2009;8:464–474. | |
ETHNICITY AND NONMOTOR SYMPTOMS IN PARKINSON’S DISEASE
So far, only very little work has been done to investigate possible variations in the motor and nonmotor profiles of patients with PD from different ethnic groups. Findings of previous studies have suggested that there might be differences of the presentation and range of motor and nonmotor symptoms in patients with PD related to ethnicity (7,8,39,63,64,65). One has to take into account several factors which might play an important role such as a possible limited access to anti-Parkinson’s drugs and the sociocultural attitude to disease management in different ethnic groups. To date, the origin and pathophysiology of these possible variations are still unclear, and robust evidence base remains an unmet need.
HOLISTIC ASSESSMENT OF NMS BURDEN IN CLINICAL PRACTICE
Till 2006, no holistic validated tools for the assessment of the multimorbid PD patient presenting with a wide range of symptoms were available. As a consequence, NMS could only be assessed selectively in clinical practice. However, to date, the measurement and self-reporting of NMS in clinical practice have been addressed by several initiatives such as the SCOPA scales (Scales for Outcomes in PD), the NMS questionnaire (NMSQuest) and scale (NMSS) as well as new version of the Movement Disorder Society–Unified Parkinson’s Disease Rating scales (66,67).
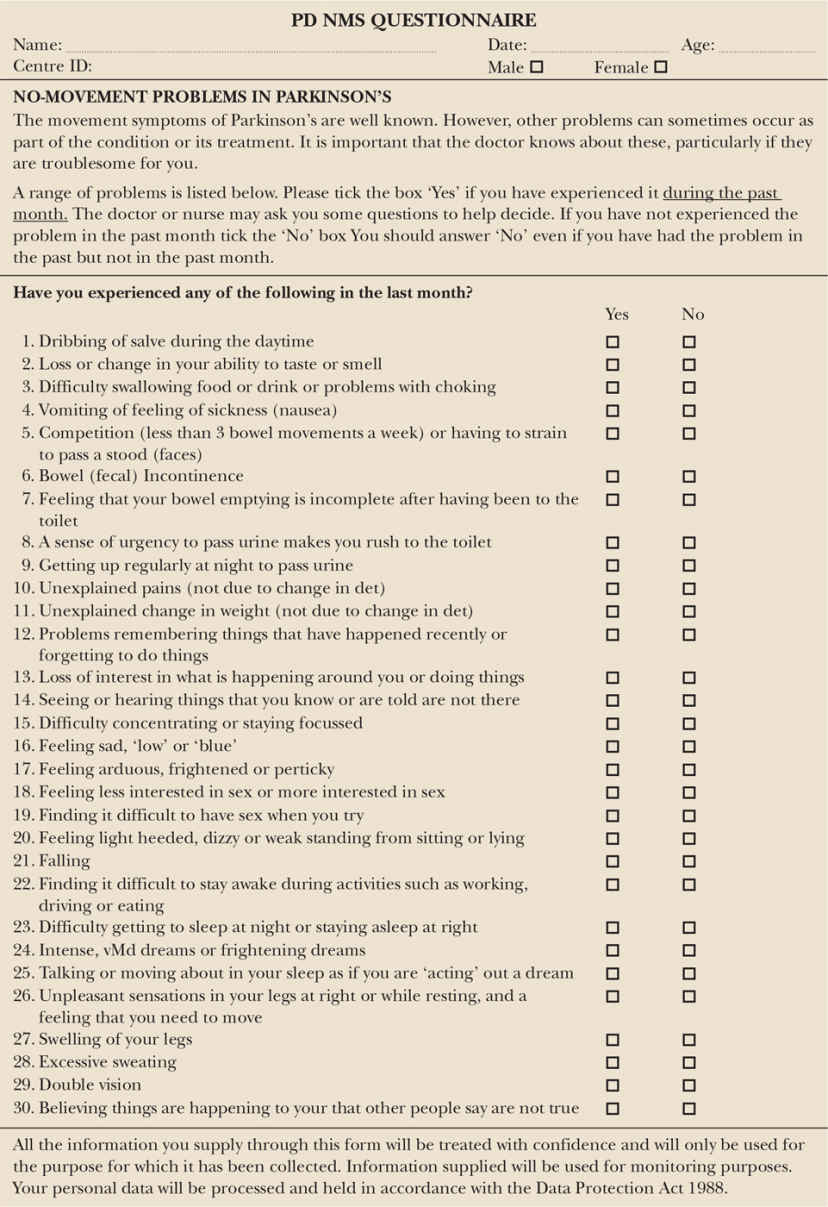
THE NMS QUESTIONNAIRE
The validated NMSQuest can be easily completed by the patient (proxy of carer allowed) in the “yes” and “no” fashion, while he/she is waiting to be seen by the health professional. As a consequence, the completion of the NMSQuest does not influence the actual consultation time and additionally gives a helpful and quick “snapshot” of the NMS burden of each individual patient during the last month.
The NMSQuest is now recommended by national and international societies for use such as the UK Department of Health, the international Movement Disorders Society, and the US National Institute of Neurological Disorders and Stroke as well as patient groups such as Parkinson’s UK.
The NMSQuest includes 30 questions covering 10 different domains ranging from gastrointestinal to miscellaneous (Fig. 6.1 and Table 6.5). As reported by a European study, more than 50% of patients do not mention or discuss the NMS they are experiencing when seeing the health professional (68). The NMSs were only considered when the clinician became aware of them after the use of the NMSQuest. The data is supported by two recent studies in de novo PD (DeNoPa study) and a study in early PD (69).
NMS SCALE
In order to quantify and grade-rate each NMS over the last month with respect to the severity and frequency, the rater (health professional) completed NMSS can be applied. The NMSS includes 30 items covering nine domains: cardiovascular (two items), sleep/fatigue (four items), mood/cognition (six items), perceptual problems/hallucinations (three items), attention/memory (three items), gastrointestinal tract (three items), urinary function (three items), sexual function (two items), and miscellaneous (four items). Each NMS is rated regarding the severity (from mild (0) to severe (3)) and the frequency (from rarely (1) to very frequent (4)). By multiplying the score of the severity and the frequency, each item can be graded. As a consequence, each item’s score ranges from 0 to 12, and the NMSS’s total score range is from 0 to 360.
< div class='tao-gold-member'>