74
Nucleus Pulposus Replacement Techniques
Jeff S. Silber and Jared F. Brandoff
Description
Techniques of selectively replacing the central nuclear portion of the diseased lumbar intervertebral disk with the goal of restoring as closely as possible the normal structural and functional properties of the native intervertebral disk have been described since the 1950s. Not until recently, however, have advances in biomaterials and mechanical testing techniques made selective nucleus replacement a feasible and viable technique.
In modern times, the gold standard of surgical management of end-stage degenerative disk disease is fusion of the diseased motion segment. To date, however, fusion procedures have yielded relatively unpredictable outcomes. Furthermore, fusion renders a patient potentially susceptible to various other morbidities, including posterior muscle atrophy, decreased motion and stiffness at the fused level, and transfer of loads leading to accelerated adjacent-level disease as well as morbidities at the bone-graft donor site associated with harvesting. Lehman et al have demonstrated that fusion leads to adjacent-level facet hypertrophy, spinal stenosis, and ultimately potential instability.
Moreover, in the case of disk herniation, partial diskectomy has been demonstrated to lead to gradual loss of disk space height over time. Removal of any significant portion of the nucleus pulposus changes the biomechanics of the remaining disk elements. In the normal intervertebral disk, axial loads are transferred through the viscoelastic nucleus pulposus to the surrounding anulus fibrosus. This leads to normal concordant out-bulging of both the inner and outer fibers of the anulus. Loss of nucleus material or loss of disk height from degenerated nucleus material leads to less efficient transfer of axial loads and discordant bulging of the inner and outer fibers of the anulus. The result is out-bulging of the outer fibers and in-bulging of the inner fibers. This disjointed bulging leads to increased exposure to shear forces within the anulus and ultimately decreased ability to resist compressive loads. In turn, this can lead to acceleration of the disk degenerative process as well as supraphysiologic transfer of loads to the facet joints posteriorly.
Conceptually, if the diseased or deficient nucleus material could be replenished with a material that exhibits the same biomechanical properties as nucleus pulposus material, then the physiologic biomechanics of the intervertebral disk could be restored. This is the goal of modern nucleus replacement technologies. These materials exhibit viscoelastic properties similar to native nucleus. They provide restoration of premorbid disk height and thus redistribution of forces during axial load. Current designs are biologically compatible, fatigue resistant (potentially withstanding 100 million cycles over a 40-year period), and resistant to the production of particulate debris. Several different designs are currently in different stages of preclinical and clinical testing. To date, however, all nucleus replacement materials and techniques are considered experimental. Significantly more research and clinical trials are required in this area.
Expectations
In the setting of degenerative disk disease, it is theoretically desirable to remove the anterior portion of the disk nucleus, which has been described as a potential pain generator, and replace the diseased disk portion with a material that exhibits similar biomechanical properties to an undiseased or healthy disk. Specifically, it is expected that nucleus replacement will retain physiologic motion of the spinal segment while simultaneously retaining the inherent stability of that segment. This, in turn, should alleviate the transfer of stress to the posterior facet joints while simultaneously tensioning the anulus to minimize further irritation to the sinuvertebral nervous network. Ideally, this can be achieved through a minimally invasive approach, thus further preserving the surrounding soft tissue stabilizers and retaining stability at the segment. The implant should allow for stable motion similar to a healthy disk. Finally, the resulting restoration of disk height will decrease shear forces on the remaining anulus, facet joints, and stabilizing ligaments.
Indications
Nucleus pulposus replacement techniques are indicated in patients with severe disability from lumbar degenerative disk disease who have failed at least 6 months of active, nonsurgical management. Imaging studies should demonstrate moderate disk degeneration with 10 to 50% loss of disk height. A lumbar provocative diskogram must demonstrate an intact anulus fibrosus, and pain provocation should be concordant with the patient’s usual low back pain. Magnetic resonance imaging (MRI) findings should be limited to an early stage of degenerative changes, including a total disk height of greater than 5 mm, absent Schmorl’s nodes, and mild facet arthrosis. Furthermore, this technique is indicated following a partial diskectomy for a disk herniation if the other aforementioned criteria are fulfilled, as a method of diminishing subsequent loss of disk height.
Contraindications
Contraindications for this technique are associated with significant, end-stage degenerative disk disease. Specifically, significant fissuring of the anulus on the diskogram or advanced degenerative changes such as severe facet arthrosis or spondylolisthesis.
Special Considerations
Available nucleus replacement implants today are either constrained or unconstrained. Constrained implants consist of an outer casing with a relatively fixed size and shape. This provides for less creep of the implant. Because of their predetermined size and shape, however, this design may not contact the entire surface of the adjacent vertebral end plates. This highlights the importance of having a compatible modulus between the implant and the end-plate bone. Incompatibility of modulus can lead to stress shielding, and, in accordance with Young’s law, can lead to bone resorption at the end plates adjacent to the implant. This can predispose the implant to ultimate subsidence or extrusion. Unconstrained implants do not have a predetermined size or shape. They are injected and swell to fill the disk space, maximally providing the maximum surface area for stress distribution. This can lead to less implant motion and potentially fewer extrusions. Some hydrogel devices are made of a co-polymer of polyvinyl alcohol (PVA) and polyvinyl pyrrolidone (PVP). The Prosthetic Disc Nucleus (PDN) implants (Raymedica Inc., Bloomington/Minneapolis, MN) are composed of an internal hydrogel co-polymer pellet of polyacrylonitrile and polyacrylamide. It can be molded into sizes and shaped to the appropriate enucleated nucleus cavity formed following a diskec-tomy. The outer constraining cover is composed of a loosely woven high molecular weight polyethylene (HMWPE). The device can absorb water up to 80% of its dry weight to help provide force to elevate the disk space. However, unconstrained hydrogels require at least 5 mm of disk height for placement and expansion. These implants are ideally injected in a fluid phase and harden in vivo to the desired size and shape of the disk defect.
Tips, Pearls, and Lessons Learned
Ideal patient selection for this technique is paramount. In patients undergoing a partial diskectomy either via a minimally invasive microdiskectomy approach with or without tubular retractor systems, placement of a nuclear replacement device may alter the natural history of continued degeneration. Technically, appropriate intervertebral preparation and proper placement of the device to avoid extrusion is key to optimizing long-term results.
Key Procedural Steps
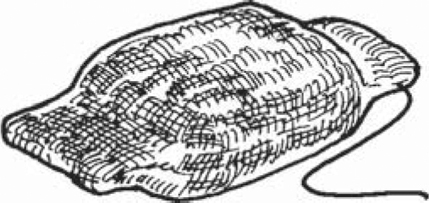
Specific procedural steps are outlined in the respective technique guides for each available implant type. Nearly all techniques employ a minimally invasive posterior approach that spares as much of the soft tissue sleeve as possible. It is recommended that laminar spreaders be used in an attempt to diminish the size of the laminotomy. The approach is similar to one performed for a microdiskectomy. A stab anulotomy is performed, and initially a smaller sized dilator is used followed by a larger one and rotated 90 degrees to stretch the outer anulus fibers. Pituitary rongeurs are used to remove the nucleus and attention is paid so as not to disrupt the anulus and vertebral end plates. A dural retractor is utilized to protect the neural elements. Once the appropriate amount of nucleus is removed, which can be checked with a probe, depth gauge, or intraoperative diskogram, the device is placed. The largest device size is chosen (constrained device), as measured with sizing instruments (Fig. 74.1). The device is placed with a flexible guide; the guide is placed into the nucleus cavity and a suture (No. 1 or 0 Vicryl) is sewn into the leading edge of the device (e.g., PDN device). The device is tamped in with an impactor following the flexible guide while pulling on the suture to help place the implant horizontally across the intervertebral disk space as best as possible (Fig. 74.2). Final positioning is confirmed with radiographic imaging (Fig. 74.3). If needed, a laminotomy and anulotomy may be performed on the opposite side to remove additional nucleus and aid in better device placement with the use of tamps and by pulling the suture attached to the leading device edge. Furthermore, when possible, it is desirable to employ anulus closing techniques, although presently none of the described techniques available today are completely satisfactory, to repair the requisite anulotomy after implant insertion. This should decrease the rate of implant extrusion. Finally, Bertagnoli has recently described a retroperitoneal trans-psoas approach that may be advantageous. It is generally advisable to avoid anterior approaches so that they may be retained for subsequent surgical intervention should the need arise.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








