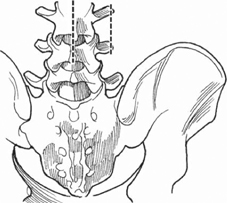
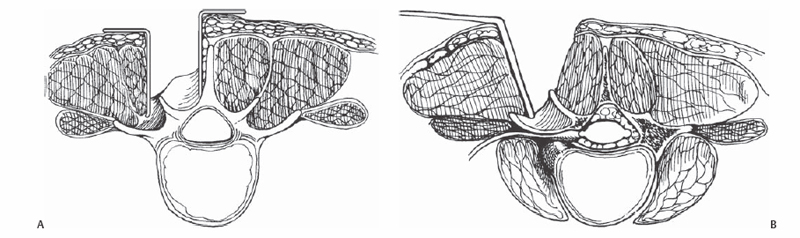
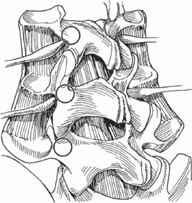
35 Ralph J. Mobbs and Charles G. Fisher A technique to access the nerve root and disk pathology lateral to the foramen for removal of a far lateral disk herniation. Midline or paramedian incision and an approach without entering the spinal canal to maintain the integrity of the facet joint and expose the nerve root (Fig. 35.1 and 35.2). Fig. 35.1 Incision options include midline or paramedian. A midline approach requires a longer incision to expose far lateral to the TP and pars; however, it will be more “familiar” anatomy. A paramedian incision will be a shorter, muscle-splitting approach. Fig. 35.2 (A,B) A midline incision results in a more painful muscle dissection and retraction combination. The paramedian incision is a more direct route to the pathology; however, it is an unfamiliar approach. A hemilaminectomy and facetectomy may lead to poor long-term results for far lateral disk herniation surgery. Adapting a method to avoid issues of mechanical instability by approaching the impinged nerve root and disk lesion from lateral to the pars/facet joint will improve outcomes. If a far lateral disk herniation is suspected on computed tomography (CT), it can be confirmed with magnetic resonance imaging (MRI), including parasagittal views. Position the patient prone on a Wilson frame, Jackson spine table, or a 90/90 Andrews frame. Use x-ray or fluoroscopy to mark out the limits of the exposure priorto skin incision, and then reconfirm when landmarks are exposed. Illumination and magnification are paramount; use either a microscope or loupe/ headlight combination. Endoscopy may be an option with tubular retraction devices.
Open Far Lateral Disk Herniation
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








