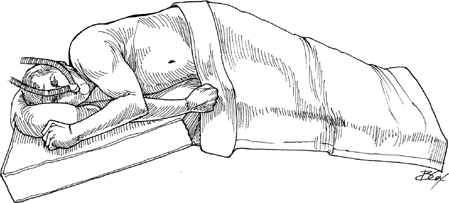
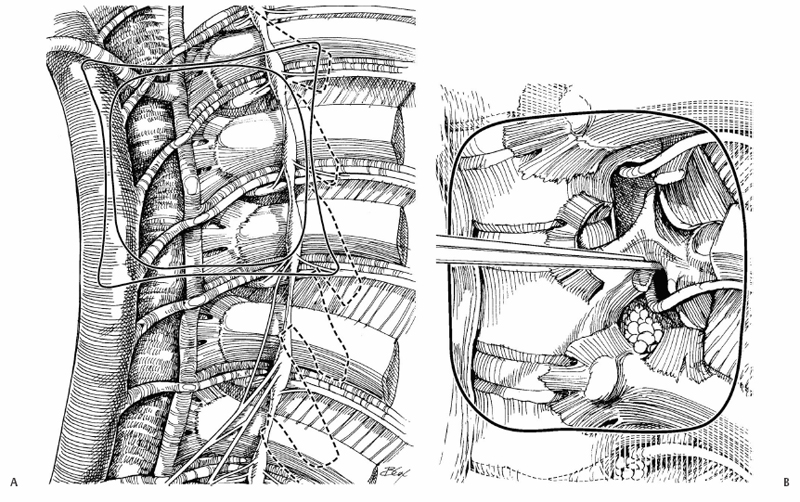
31 James D. Kang and Mustafa H. Khan Access to the anterior thoracic spine is used for decompression and fusion. Obtaining good exposure is the most important factor in performing adequate decompression of the neurologic elements of the thoracic spine. Depending on the level of thoracic spine, special consideration should be given to preserve vascular structures and thoracic/abdominal viscera. The transthoracic approach offers excellent visualization of the anterior thoracic spine for decompression and fusion. Burst fractures with canal compromise and neurologic deficit, large extruded thoracic disks with cord impingement, intraspinal tumors, infections. Severe pulmonary disease, medical comorbidities such as severe cardiac disease, posterior spinal instability without intent to perform a posterior adjunctive procedure. Preoperative workup should include imaging modalities (plain radiographs, magnetic resonance imaging [MRI], or computed tomography [CT] scan) to specifically define the area of decompression. If a tumor is being evaluated, CT angiography and embolization are helpful in preoperative planning. A thoracic surgery consultation for exposure and intraoperative assistance can be useful. Intraoperative somatosensory or motor evoked potentials should be used to monitor the cord. The patient is placed in a lateral decubitus position with the operative side (right or left, depending on the thoracic level) up (Fig. 31.1). The table is flexed to open up the intercostal intervals before beginning the approach. Magnifying loupes and head lights are helpful. We prefer to use a double-lumen endotracheal tube to deflate one lung. A nasogastric (NG) tube may be used for identifying the esophagus intraoperatively. Fig. 31.1 The patient is placed in the lateral decubitus position. In general, many surgeons prefer a left-sided approach. The level of entry between ribs depends on the level of pathology; it is better to err in the cephalad direction than in the caudad direction. A right-sided approach to T11-L1 may place the liver at risk. Access to the T2 and T3 vertebral bodies via a thoracic corpectomy is technically challenging; a sternal splitting approach may be easier. The other option is a very high periscapular thoracotomy, performed via excision of the fourth rib. Ligation of segmental vessels is useful for maintaining good hemostasis. On the left side the artery of Adamkiewicz is at risk between T9 and T12. It is advisable not to tie off those vessels initially but rather to clamp them individually and watch for any somatosensory evoked potential (SSEP) signal changes. The blood supply to the spine via segmental vessels is highly variable. Also, exposing the wrong interspace and having to work cephalad for the appropriate exposure makes surgery more difficult. During left-sided approaches the thoracic duct is at risk for injury. The aorta and inferior vena cava are almost always visible in the surgical field. The hemiazygous and azygous systems are vulnerable to injury especially high in the thoracic spine. This is important because placement of anterior instrumentation under the aorta may lead to late aortic erosion and catastrophic aortic rupture. Some patients (especially those with severe lung disease) cannot tolerate unilateral lung deflation. Care must be taken not to puncture visceral pleura. Finally, inadequate decompression of the vertebral bodies may result if decompression is not carried all the way to the far pedicle. A thoracotomy incision is made at the level corresponding to the vertebral level to which access is being sought. In large or obese patients, it may be difficult to identify the appropriate intercostal rib space to enter. Intraoperative plain radiographs with a spinal needle can help with the identification of the levels, but, in general, it is better to err on the more cephalad level because it is technically easier to perform the corpectomy working cephalad to caudad rather than vice versa. Care is taken to perform the dissection of the rib on its superior border to avoid damage to the intercostal nerve and vessels, which run along the inferior border. The dissection is carried down into the thoracic cavity by incising the pleura. A self-retaining rib-spreader is placed between the cephalad and caudad ribs. It is often necessary to resect the rib to allow for better retraction; otherwise, it is not uncommon to fracture the ribs with the rib spreading retractors. The lung is deflated via the double-lumen tube. Within the chest cavity, the rib that corresponds to the vertebral body that will be removed with the corpectomy is followed posteriorly to the spine where it articulates at the cranial border of the vertebral body and the intervertebral disk (e.g., the 8th rib articulates into the T7-8 disk space). It is strongly advisable at this time to obtain a confirmatory plain radiograph with a spinal needle to check that the levels have been counted correctly. The parietal pleura is resected, making a rectangular window over the vertebral body and the rib heads (Fig. 31.2). The segmental vessel is ligated to fully expose the lateral bony wall of the vertebral body, which is to be removed. The sympathetic chain is often encountered and may be ligated to enhance full exposure of the vertebral body and the adjacent disks. The rib head is now disarticulated to allow for exposure of the pedicle (the rib can be saved for use as bone graft). It is also important to remember that the rib head articulates with the transverse process (costotransverse articulation) as well as the vertebral body (costovertebral articulation), and good exposure of the pedicle requires complete resection of these structures.
Open Thoracic Corpectomy via the Transthoracic Approach
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







