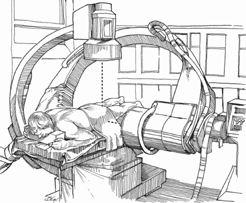
66 Choll W. Kim and Steven R. Garfin Percutaneous vertebral augmentation (vertebroplasty, kyphoplasty) is used to treat painful vertebral compression fractures due to osteoporosis or lytic tumors via injection of bone cement into the vertebral body. Immediate stabilization of vertebral body fractures to decrease pain or prevent further collapse of the vertebral body. Fracture reduction can be obtained in some circumstances using postural techniques or with the use of an inflatable bone tamp (kyphoplasty). Patients with painful vertebral compression fractures may have severe pain for prolonged periods of time. This treatment provides a minimally invasive method of stabilizing the micromotion of the fracture and thereby decreasing pain. Pain relief occurs within 1 or 2 days in most cases. Pain relief has been correlated with fracture reduction. However, fracture reduction via kyphoplasty is best accomplished when fractures are treated within 2 to 3 months. Percutaneous vertebral augmentation is indicated for the treatment of painful, low-energy thoracic and lumbar vertebral body fractures due to osteoporosis and certain lytic lesions, such as multiple myeloma. Percutaneous vertebral augmentation should not be used in the setting of infection and certain massoccupying lesions, including solid tumors and arteriovenous malformations. This technique is intended to stabilize the micromotion associated with low-energy fractures. It is not recommended in high-energy injuries with concomitant ligamentous or posterior element injuries. Care should be taken in vertebral body fractures with posterior wall involvement (discussed later). The proper identification of the painful vertebrae can be challenging. In addition to radiographs, advanced imaging studies must be obtained. Magnetic resonance imaging (MRI) is the most useful method of evaluation. Technetium bone scan is useful in patients with a contraindication to MRI, such as brain aneurysm clips or cardiac pacemakers. Clinical localization of the fracture using percussion of the spinous processes can be helpful in distinguishing distant sites (e.g., T6 versus L4), but not nearby sites. The posterior wall is often involved, but is not always an absolute contraindication to vertebral augmentation. In low-energy injuries with an intact posterior longitudinal ligament, the cement is often prevented from entering the canal. A secondary indicator of posterior wall compromise is the presence of an epidural hematoma. This suggests that the fracture communicates directly with the epidural space and thus may be a conduit for cement leakage. Percutaneous vertebral augmentation should be pursued only with great caution. Vertebral compression fractures may be caused by pathologic conditions such as tumor or infection. Unless the diagnosis of osteoporosis is well established, a biopsy is recommended. In patients who have a dual-energy x-ray absorptiometry (DEXA) study consistent with osteoporosis, no history of malignancy, and a previously known osteoporotic vertebral compression fracture, a biopsy is not necessary. Gentle lordotic positioning allows some postural reduction in certain fractures. The procedure can be performed with local anesthetic in many patients. The patient should be able to lie prone for at least 1 hour without significant pain or respiratory difficulties. Attention to injecting the periosteum of the entry point decreases pain during trocar insertion. Some pain may be encountered during balloon inflation or during injection. This is best treated with reassurance and gentle intravenous sedation. If general anesthesia is utilized, the patient must be handled gently. Rib fractures may occur as a result of undue pressure in the course of patient positioning and during impacting maneuvers to insert the trocar into the vertebral body. The use of biplanar fluoroscopy greatly aids cannula insertion and cement injection. Biplanar fluoroscopy is readily obtained by using two separate C-arms (Fig. 66.1). The lateral image is brought over the top and the arc, leaning away toward the head. The anteroposterior (AP) image is brought in diagonally with the image intensifier directly over the target site. It is most convenient to obtain the true AP image first because the diagonal entry makes this process challenging. The lateral image is then adjusted around the AP image. Meticulous attention should be exercised to obtain true AP and lateral images of the target vertebrae.
Percutaneous Cement Augmentation Techniques (Vertebroplasty, Kyphoplasty)
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







