Primary and Secondary Stroke Prevention
Charles C. Esenwa
Mitchell S. V. Elkind
INTRODUCTION
Prevention of stroke can be divided into three types: (1) primordial prevention, which focuses on improving community-wide health behaviors, such as diet, exercise, and smoking; (2) primary prevention, which attempts to mitigate an individual’s stroke risk factors; and (3) secondary prevention, which targets risk of stroke recurrence in those who have already suffered a stroke or transient ischemic attack (TIA).
Risk factors are generally classified as either nonmodifiable or modifiable. Nonmodifiable risk factors, although they cannot be altered, remain important in quantifying a patient’s future risk of stroke. Examples include age, sex, family history, ethnicity, and race. Modifiable risk factors allow for intervention to decrease future risk of stroke.
Although primordial prevention deals with population-level risk of cardiovascular disease, individualized prevention measures require a careful history and tailored diagnostic evaluation to stratify stroke risk and guide the appropriate prevention strategy. Primary and secondary prevention methods both focus on improving the individual’s risk factor profile, and secondary prevention methods further depend on the mechanism of the stroke. For ischemic stroke, these mechanisms include atherothrombotic, small vessel (or “lacunar”), cardioembolic, and cryptogenic; the last is responsible for up to 40% of strokes. Several randomized controlled trials have been conducted over the past four decades that have determined optimal therapy for stroke prevention and treatment, especially for atherothrombotic and cardioembolic stroke subtypes.
Hemorrhagic strokes account for 15% to 20% of all strokes and are further divided into subarachnoid hemorrhage (SAH) and intracerebral hemorrhage. Causes of SAH include trauma, berry or congenital aneurysms, and less often arteriovenous malformations. Intracerebral hemorrhage is most commonly caused by hypertension. Appropriate classification of a stroke and its etiology aids the clinician in determining the most effective prevention strategy.
The INTERSTROKE case-control study among 22 countries determined that 10 risk factors accounted for nearly 90% of strokes. Listed in order of significance, they are as follows: hypertension, cardiac disease, current smoking, waist-to-hip ratio, poor diet, sedentary lifestyle, excessive alcohol intake, diabetes mellitus, depression, and psychosocial stress. The highest burden of stroke in the United States falls in the so-called stroke belt located in the southeast, where high prevalences of diabetes, hypertension, and obesity remain likely important drivers of cerebrovascular disease.
PRIMORDIAL STROKE PREVENTION
DIET
The Mediterranean diet may protect against cardiovascular disease, including stroke. It is characterized by high intake of fruits, vegetables, and legumes; olive oil as the principal source of fat; moderate consumption of fish and poultry, with minimal intake of red meat and dairy; and an option of mild to moderate consumption of red wine, mostly with meals. Compared to a low-fat diet, this complex combination of nutrients decreased 5-year stroke risk by approximately 30% in a prospective study. In general, any diet aimed at promoting cardiovascular health, such as the Mediterranean diet or the Dietary Approach to Stop Hypertension (DASH) diet, revolves around the central notions of a high intake of plant-based nutrients, low-salt intake, and a curbing of saturated fats and simple sugars.
SMOKING
Tobacco use is strongly discouraged and among smokers, cessation of smoking leads to a reduction in stroke risk to levels similar to nonsmokers by 5 years.
EXERCISE
Physical activity is associated with a reduced risk of stroke and, importantly, several studies provide evidence that only a moderate level of activity is required, and so physical activity should be encouraged even among the elderly. A sedentary lifestyle, in combination with consumption of simple carbohydrates, has contributed to one-third of Americans becoming obese and to even more becoming overweight. Obesity is an independent risk factor for stroke, even after adjusting for physical activity and diet. Obesity is comorbid with diabetes, hypertension, and heart disease, moreover.
PRIMARY STROKE PREVENTION
Like primordial stroke prevention, primary stroke prevention aims to limit the risk of first-time stroke, but instead of dealing with groups of people, the health care provider focuses on each individual separately. Specific targets for intervention are a person’s major modifiable risk factors including hypertension, diabetes mellitus, hypercholesterolemia, atrial fibrillation, and medication use. Several randomized trials have demonstrated the benefits of specific interventions to prevent a first stroke among patients with certain stroke risk factors (Table 44.1).
TABLE 44.1 Evidence-Based Primary Stroke Prevention | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
HYPERTENSION
Blood pressure is the most important contributor to stroke incidence, increasing the risk of stroke in a linear fashion. High blood pressure accounts for 35% of all strokes. β-Blockers, thiazide diuretics, angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), and calcium channel blockers are the most widely studied agents in stroke prevention. Although calcium channel blockers may provide the greatest neurovascular protection, they are also associated with an increased risk of heart failure. The general consensus is that protection against stroke depends on the level of blood pressure control rather than on the specific class of medication used. Blood pressure reductions of 10 mm Hg systolic or 5 mm Hg diastolic have been shown to reduce risk of first-time stroke by more than 40% [Level 1].1 In the United States, efforts targeting hypertension have contributed to the steady decline in stroke incidence and stroke-related mortality in the last half century.
The effects of adequate blood pressure management may be more robust in those with diabetes mellitus. ACEIs and ARBs are recommended because they have been proven renoprotective and also effective in reducing cardiovascular events and specifically stroke in those with diabetes mellitus.
DIABETES MELLITUS
Epidemiologic studies show a positive relationship between hyperglycemia and stroke incidence, but aggressive management of hyperglycemia may actually be harmful. The Action to Control Cardiovascular Risk in Diabetes (ACCORD) study compared intensive glucose-lowering therapy with a goal glycated hemoglobin level below 6% versus glycated hemoglobin goals of 7% to 7.9% and found no difference in stroke incidence with a slight, but statistically significant, increase in overall mortality in the group undergoing tight control. Similarly, postprandial hyperglycemia and glycemic variability have both been associated with increased cardiovascular disease burden in epidemiologic studies, but prospective studies have not shown any benefit. Current recommendations are for a glycated hemoglobin goal of less than 7%.
The presence of diabetes also has ramifications for the management of other risk factors, specifically low-density lipoprotein (LDL) cholesterol. Diabetes is considered a cardiovascular disease equivalent and those 40 to 75 years of age with diabetes should be placed on a hydroxymethylglutaryl-coenzyme A (HMG-CoA) reductase inhibitor or statin, unless there is a contraindication.
HYPERCHOLESTEROLEMIA
Large epidemiologic studies, such as the Multiple Risk Factor Intervention Trial (MRFIT) that included over 350,000 men, have shown a positive association between death from ischemic stroke and increased cholesterol levels. There has also been evidence of a relationship between hemorrhagic strokes and low cholesterol levels. In line with the MRFIT data, trials using HMG-CoA reductase inhibitors among cardiac and other high-vascular disease risk patients have demonstrated benefits in terms of stroke risk reduction, in addition to the effects on cardiac event rates. The effect on stroke risk is more modest, however, probably reflecting the fact that stroke is more heterogeneous than heart disease and less strongly linked to elevated cholesterol levels.
In the Heart Protection Study (HPS), a randomized multicenter, placebo-controlled trial of simvastatin therapy, there was a 25% risk reduction for stroke (from 5.7% to 4.3%; P <.0001), without an increase in risk of hemorrhagic stroke over a 5-year period. Importantly, these benefits remained in those with LDL less than 100 mg/dL.
Evidence suggests that the optimal way to think about cholesterol goals within the context of primary stroke prevention is to consider the individual’s long-term absolute risk of combined cardiovascular events. The Pooled Cohort Risk Assessment Equations was developed by the American College of Cardiology and American Heart Association using data from several large epidemiologic studies to predict a 10-year risk of cardiovascular events and identify appropriate candidates for statin therapy. Those with a high risk of cardiovascular events (considered to be at least 7.5% over 10 years) should be placed on cholesterol-lowering therapy, independent of specific risk factors. Other high-risk groups that should receive statin therapy are individuals with an LDL greater than 190 mg/dL and those aged 40 to 75 years with comorbid diabetes mellitus [ Level 1].2
ATRIAL FIBRILLATION
Atrial fibrillation is the most important cause of embolic stroke. Anticoagulation is effective in preventing both incident and recurrent strokes in patients with atrial fibrillation [Level 1].3 In the Stroke Prevention in Atrial Fibrillation (SPAF) study, anticoagulation reduced stroke recurrence substantially, even in patients older than the age of 75 years. Chance of embolization is associated with the following risk factors: age older than 75 years, previous embolization, sustained hypertension, and congestive heart failure. With one risk factor, the stroke incidence is nearly 3% per year and increases to 18% when all are present.
Warfarin, a vitamin K antagonist, is associated with a 60% to 70% relative risk reduction in stroke. More recently, two other classes of anticoagulant therapies have been employed: direct thrombin inhibitors and factor Xa inhibitors. Large randomized clinical trials that have compared warfarin to either dabigatran, rivaroxaban, or apixaban have shown similar or slightly better efficacy with the newer agents. Some of the trials also indicate a lowered risk of intracranial hemorrhage with less need for serum monitoring, although the role of serum monitoring for some agents is still under investigation. There are two deterrents to physicians routinely prescribing the newer agents, however. The first is the lack of a standardized clotting assay, such as the international normalized ratio (INR) for warfarin, that allows for rapid evaluation of level of anticoagulation, and the second is the lack of an effective antidote, such as fresh frozen plasma and vitamin K, that can be employed when major bleeding occurs. Current research is directed at addressing these concerns.
CAROTID STENOSIS
Another major source of preventable cerebral infarction is largevessel atherosclerotic disease and specifically internal carotid artery stenosis. In asymptomatic patients with greater than 60% carotid stenosis and low perioperative risk, carotid endarterectomy (CEA) should be considered with the expectation that approximately 20 procedures must be performed to prevent one stroke over a 5-year period. Men are much more likely to benefit than women, which, along with the patient-specific perioperative risk, helps the clinician decide whether or not to recommend surgery. Although CEA is the gold standard, carotid artery stenting (CAS) is an alternative and may be employed if the anatomy is unfavorable to surgical intervention. There is no benefit of either procedure in patients with less than 50% stenosis or in chronic carotid occlusion.
SECONDARY STROKE PREVENTION
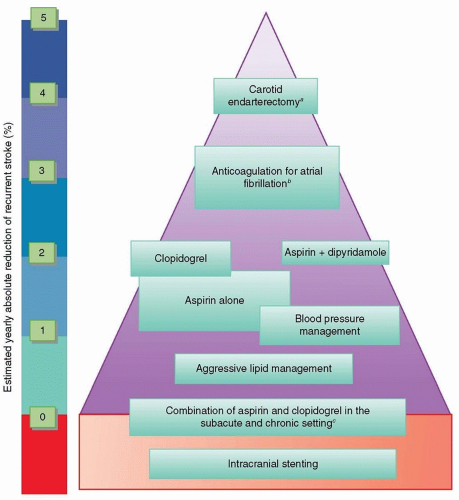
Once a stroke or TIA has occurred, the goals of the clinician are to minimize long-term disability and direct management to prevent another stroke (Fig. 44.1). Secondary stroke prevention measures do not alter progression of the initial stroke, but research has shown that initiating preventive therapy in the acute setting after stroke increases the likelihood of preventive therapy being in place in the long term.
STROKE MECHANISM AND EVALUATION
Therapies aimed at limiting risk of recurrence depend in large part on the mechanism of the stroke, its severity, and the individualized modifiable risk factor profile. Because the risk of a repeat stroke is highest in the first 2 weeks after the initial event, a comprehensive evaluation must be employed as soon as possible to determine stroke mechanism and quantify the underlying risk factors. The importance of a good history and physical examination cannot be overstated and should be followed by hypothesis-driven diagnostic testing. Magnetic resonance imaging (MRI) of the brain visualizes acute ischemic injury and can aide in determining the mechanism. Although lacunar strokes, or deep punctate infarcts within the white matter, predominantly occur from small-vessel disease, for example, large wedge-shaped infarcts or multifocal infarcts are more consistent with embolism. Extracranial vessel imaging specifically looking at the patency of the carotid arteries is a crucial step in the diagnostic algorithm, whereas intracranial vessel imaging in the form of magnetic resonance angiography (MRA) or computed tomography angiography (CTA) may be useful to identify intracranial stenosis. The gold standard for carotid imaging is digital subtraction angiography, but it is impractical for screening purposes. Carotid Doppler has therefore become the main screening test for carotid atherosclerosis, whereas the widespread availability of MRA and CTA provide alternatives to be used at the clinician’s discretion and to confirm the findings on ultrasound.
Transthoracic echocardiography is used to assess structural cardiac abnormalities that predispose to cardioembolism. In cases with a high pretest probability of embolism, transesophageal echocardiogram can be used to better visualize the left atrium and cardiac valves, looking for intra-atrial thrombus, cardiac myxoma, or valvular vegetations. A second arm of the cardiac evaluation assesses the cardiac rhythm for evidence of atrial fibrillation. Electrocardiography and cardiac telemetry are used in screening, whereas prolonged monitoring for several weeks to months can be very helpful in capturing occult atrial fibrillation. Measuring LDL, highdensity lipoprotein, hemoglobin A1c, and in appropriate or otherwise unexplained cases, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), or rapid plasma reagin (RPR) allow for proper management and prevention of recurrent stroke.
PREVENTION EARLY AFTER ACUTE STROKE
It is important to recognize that TIAs call for the same urgency in evaluation as MRI-proven strokes. Johnston et al. showed that
the risk of stroke after TIA is about 5% in the first 2 days and 10% within 90 days. Further, 1 in 20 individuals will suffer a fatal or disabling stroke within 90 days after TIA. Recent trials proved that urgent evaluation and directed management of TIA or minor stroke dramatically decreases the recurrence rate of stroke.
the risk of stroke after TIA is about 5% in the first 2 days and 10% within 90 days. Further, 1 in 20 individuals will suffer a fatal or disabling stroke within 90 days after TIA. Recent trials proved that urgent evaluation and directed management of TIA or minor stroke dramatically decreases the recurrence rate of stroke.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree