24 Spinal Infections Eli M. Baron, Joshua E. Heller, Christopher M. Loftus, and Alexander R. Vaccaro Spinal infections represent a serious source of morbidity and mortality for patients. Even with modern-day treatment modalities, including surgical debridement, spinal reconstruction, and antibiotic therapy, a mortality rate of 20% has been reported in some variants of spinal infection.1 This chapter reviews pyogenic and nonpyogenic infections of the spine as well as postoperative wound infections because these may be considered the most common spinal infections requiring surgery. Excluded from this discussion are infectious entities that may involve the spinal cord or its coverings that are generally treated medically, such as human immunodeficiency virus (HIV)-related myelopathy and meningitis. Spinal infections can be classified as pyogenic versus nonpyogenic.2 Pyogenic spinal infections refer to infections of the spine resulting in purulence and predominantly a neutrophilic response.3 These are typically caused by bacteria but may also occur as a result of parasitic or fungal organisms. Nonpyogenic infections result in a granulomatous response and are usually caused by mycobacteria, parasites, or fungi.4 Spinal infections can also be categorized by their anatomical location in relation to the spinal column, dura, and spinal cord. Osteomyelitis refers to infection of the vertebrae or bone of the spine. Alternatively, this is referred to as infectious spondylitis. Diskitis refers to infection of the disk space. Combined infection of the disk and adjacent bone is referred to as spondylodiskitis. Septic arthritis of the facet joint may be seen in isolation or in combination with adjacent osteomyelitis or epidural abscess.5–10 Epidural abscess can be seen alone but is usually seen in combination with diskitis or spondylodiskitis. Subdural infection is much more rare but has been reported.11,12 Intramedullary abscess of the spinal cord may also be seen.13–18 The most common organism seen causing pyogenic infections is Staphylococcus aureus (~60% of infections) followed by Enterobacter (30%). Less commonly Salmonella, Klebsiella, Pseudomonas, and Serratia are involved.4 Epidural abscess is caused most often by Staphylococcus aureus (63% of cases). Most cases involve methicillin-sensitive Staphylococcus aureus (MSSA) species; however, cases of methicillin-resistant S. aureus (MRSA) infections do occur. Other less common causative bacteria are Streptococcus species, Pseudomonas, Escherichia coli, and Lactobacillus. Mixed flora with combinations of the foregoing organisms also occurs, as well as infection with oral flora such as Prevotella oris and Peptostreptococcus micros.19–23 Nonpyogenic infections of the spine are most commonly caused by Mycobacterium tuberculae followed by Brucella species. Fungal pathogens are seen in normal hosts and immunocompromised hosts. Those seen in normal hosts include Blastomyces dermatitis, Coccidioides im-mitis, and Histoplasma capsulatum, whereas opportunistic fungi, including Aspergillus, Candida, Cryptococcus, and Mucor, are seen in immunocompromised hosts.4,24 Reports of other unusual fungal organisms such as Sce-dosporium (Pseudallescheria) species causing vertebral osteomyelitis also exist.25,26 Echinococcosis, onchocerciasis, toxoplasmosis, toxocariasis all can cause nonsuppurative spondylodiskitis.4 Taenie solium, the causative agent of cysticercosis, may cause epidural, subarachnoid, or intramedullary spinal infection.27–33 Nocardial species have also been reported to cause nonpyogenic spondylodiskitis and epidural abscess.34–37 Pyogenic spinal epidural abscess is a relatively rare condition. The incidence of this potentially devastating infection appears to have increased in recent years. Current best estimates of incidence in the United States is two hospitalizations per 10,000,19 higher than original estimates of two to 25 patients per 100,000.21,38 Spinal epidural abscess occurs most commonly in males over the age of 30 with most patients being in their sixties. The male-to-female ratio in epidural abscess is 2.5:1.23 Epidural infection in the pediatric population is very unusual, though rare case reports exist.39 Probably the most frequent risk factor for spinal epidural abscess is intravenous drug use (27% of cases).19 Additional risk factors are listed in Table 24-1.40 Nonspinal infections may lead to epidural abscess via hematogenous spread or by direct extension. Cellulitis can lead to hematogenous seeding of the epidural space, whereas retropharyngeal abscess, often after surgery (21% of cases), can extend directly posteriorly leading to osteomyelitis and epidural abscess. Diabetes mellitus is a well-known risk factor for the development of infection and is identified in ~20% of cases. Disease states and therapies that lead to an immunocompromised state such as HIV, malignancy, and chronic steroid use also predispose patients to the development of epidural abscess.19 Hemodialysis and indwelling catheters (which often become infected) can predispose patients with end-stage renal disease to the formation of epidural abscesses, often with MRSA.41–43 Other important risk factors include preexisting or synchronous nonspinal infections and spine trauma.19,23
Classification
Organisms
Risk Factors, Epidemiology, and Pathophysiology
| Potential Source of Infection | Local Vertebral Predisposing Factor | Systemic Condition |
| Skin infection | DJD | Diabetes mellitus Alcoholism |
| Vertebral osteomyelitis/diskitis | Spondylosis | Liver cirrhosis |
| Pulmonary/mediastinal infections | Previous spinal operations | Chronic renal insufficiency |
| Sepsis | Previous spinal trauma | Crohn’s disease |
| Urinary tract infection | Epidural anesthesia | SLE |
| Paraspinal abscess | Paravertebral injections | Neoplasm |
| Pharyngitis | Lumbar puncture | Immunodeficiency syndrome |
| Wound infection | Advanced age | |
| Endocarditis | ||
| Upper respiratory tract infection | ||
| Sinusitis | ||
| HIV infection | ||
| Soft-tissue infection | ||
| Intravenous drug abuse | ||
| Vascular catheter |
Source: Adapted with permission from Bremer AA, Darouiche RO. Spinal epidural abscess presenting as intra-abdominal pathology: a case report and literature review. J Emerg Med 2004;26:51–56.
DJD, degenerative joint disease; HIV, human immunodeficiency virus; SLE, systemic lupus erythematosus.
Spinal epidural abscess after epidural steroid injection has been described but its incidence is very low, estimated at one case per 70 to 400,000. More commonly, epidural abscess develops following infection of indwelling catheters such as those used in epidural anesthesia.44 Recent spinal trauma has also been identified as a risk factor for the development of epidural infection. It is theorized that blunt trauma leads to a focal area of decreased immunologic resistance facilitating the implantation of infection by a hematogenous route.23
Spinal epidural abscesses most commonly occur in the lumbar spine, followed by the thoracic spine, where they are usually confined to one or two levels.23 They are often associated with either or both vertebral osteomyelitis and diskitis.3 The most common organism seen in one series was S. aureus, followed by Mycobacterium tuberculosis, Escherichia coli, and Staphylococcus epidermidis.23
Vertebral osteomyelitis represents roughly 2% to 7% cases of osteomyelitis and in developed countries ranks third in frequency only to femoral and tibial osteomyelitis.44 Given its relative rarity, and often nonspecific presentation, diagnosis is often delayed. Additionally, given the common presentations of neck or back pain, and nearly universal occurrence of these symptoms in the general population, the diagnosis is often delayed for weeks to months.46–48 Pyogenic vertebral osteomyelitis appears to be on the rise. This is probably due to an increase in the elderly population and the immunocompromised population, including HIV and intravenous drug abuse. Additionally, more invasive diagnostic and therapeutic medical procedures may be associated with pyogenic infections, especially urological procedures. Concurrent infection of the skin, respiratory tract, or genitourinary tract is often seen as a source of spinal infection and may be present in roughly 40% of patients who have vertebral osteomyelitis.49 Other common risk factors include intravenous drug abuse, which occurs in roughly 40% of cases, diabetes mellitus in 10% to 30% of cases, and concurrent medical illness in 20% to 23% of cases.49–51
The pathophysiology of pyogenic osteomyelitis and diskitis remains uncertain. Controversy exists as to the precise route of infection spread. Although local diskitis usuallyoccurs in children and young adults, primary involvement of the vertebrae is significantly more common in adulthood.46 Given the highly vascular nature of the intervertebral disks in children, where there is direct profusion of the nucleus pulposus, the blood supply may be a source of hematogenous seeding of the disk. In a mature spine, however, the vasculature is limited to the anulus fibrosus. Thus, in the adult, the initial infection may start in the metaph-ysis of the vertebral body, with subsequent spread to the disk space.52
In terms of organisms, S. aureus is the most common organism seen with vertebral osteomyelitis, accountable for 50% to 65% of cases. Additionally, S. aureus was responsible for nearly all osteomyelitis cases in the preantibiotic era.45,53,54 Less commonly, other organisms are seen, including E. Coli and other enteric bacteria.
Intramedullary spinal cord abscess is significantly rarer than the foregoing entities. Since 1950, an average of one case per year has been reported in the literature. Intramedullary abscess seems to occur with a male preponderance and a mean age of 28.9 years and most commonly involves the thoracic cord.55 Usually, abscesses occur secondary to a primary focus of infection. More common foci of infection associated with intramedullary abscess include pneumonitis, genitourinary tract infection, skin infections, endocarditis, and meningitis. Immunocompromised state is also a risk factor.56,57 There is also an association with dermoids, epidermoids, infected dermal sinus tracts, and dys-raphism.55,58–60
Typically, intramedullary abscesses start in the gray matter and extend into the white matter. Afterward the infection may extend rostrocaudally, separating fiber tracts.55 Organisms may enter the spinal cord via a variety of routes, including hematogenous spread, septic emboli, and contiguous spread from an adjacent infection or by continuity with an infected dermal sinus tract.
Tuberculosis of the spine, also known as Pott’s disease, had decreased markedly in incidence in developed countries with the advent of improved treatment. Since the 1980s, however, there appears to be an increase in incidence, largely due to its association with HIV. The majority of cases of Pott’s disease are likely hematogenous in origin, with an original pulmonary focus.61 Spinal tuberculosis (TB) represents 1% of all TB infections and 25% to 60% of all osteomyelitis and joint infections caused by Mycobacterium tuberculae.4,62 Lower thoracic and lumbar vertebrae are most frequently involved, whereas the sacrum and cervical region are involved less frequently.63
Brucellosis of the spine occurs in 2% to 30% of all cases of brucellosis with bone involvement.63 Brucellosis is a zoonotic infection that occurs most commonly among farmers, veterinarians, dairy workers, and other people working with grazing domestic mammals.4 Spinal involvement occurs more frequently in the elderly and is either focal or diffuse and usually occurs in the lumbar region, although cervical or thoracic involvement is usually associated with more neurological deficits.64
Fungal spinal infections also tend to be more common in immunocompromised hosts and usually result from hematogenous seeding.47,65,66 Nevertheless, as mentioned earlier, certain regional endemic fungi may affect immunocompetent hosts and, rarely, may result in spinal infection. Coccidioides immitis infections are endemic to the dry soil of the American Southwest and Central and South America, and its disease prevalence is increasing. One hundred thousand new infections are diagnosed yearly, of which 34% are symptomatic. Among symptomatic individuals, 5% to 10% will develop a serious pulmonary infection, and of those that have a serious infection, less than 1% will develop either or both chronic pulmonary disease and extrapulmonary dissemination including spinal involvement.67Histoplasma capsulatum is endemic to Missouri and the Ohio and Mississippi River valleys and usually causes a benign and self-limited disease. Normal host defense mechanisms tend to limit or prevent disseminated spread from its initial pulmonary focus. When disseminated histoplasmosis occurs, only very rarely does it cause an intramedullary abscess.68 Other Histoplasma species have been reported to rarely cause spondylodiskitis.69–71 Blastomyces dermatitidis is a dimorphic fungus endemic to the soil of the Mississippi and Ohio River basins and also midwestern states that border the Great Lakes. Infection has also been reported in Central and South America, Africa, and the Middle East. Infection likely occurs by inhalation of conidia. Extrapulmonary dissemination may occur, with the skin being the most common site of involvement.24 Osseous involvement may occur in as many as 10% to 60% of those patients with disseminated disease.72 When it occurs in the spine, it most likely causes a spondylodiskitis in the lower thoracic or lumbar spine, where the anterior vertebral body is affected initially.24
Pathogenic fungi that typically invade immunocompromised hosts include Cryptococcus, Candida, Aspergillus, and Mucor species. These exist worldwide. Cryptococcus is found in soil and pigeon feces and is common among patients with HIV and among organ transplant recipients. Infection is usually acquired by inhalation. Spread is usually hematogenous.24 Roughly 5% to 10% of patients with cryptococcal infection will have spinal vertebral involvement wherein the lumbar spine is most frequently involved, followed by the cervical spine.73,74 Aspergillus spores are typically found in water, soil, decaying plant matter, and grains. Like the other fungi, infection most commonly occurs by hematogenous spread, usually from the lungs. Aspergillus vertebral osteomyelitis is similar to pyogenic vertebral osteomyelitis in that there is a male preponderance, usually the lumbar spine is involved, and the most common symptom is back pain. Candida species are among the normal flora of the gastrointestinal tract and skin and female genital tract.24 The lower thoracic or lumbar spine is most frequently involved.75
Parasitic infection may also occur in the spine. Echinococcus species are found worldwide living within the intestines of carnivorous mammals, their ova being passed with stool. Subsequently, intermediate hosts such as livestock ingest the ova, which hatch in the duodenum. These embryos reproduce asexually, forming multiloculated cysts. Human infection occurs when contact with ova occurs through contaminated food or direct contact with feces. Osseous involvement with hydatid cyst disease is unusual, but when it does occur it involves the spine 44% of the time.76 Spinal infection most likely occurs through vertebral-portal venous anastomosis.77 Spinal infection with Echinococcus can occur as primary intramedullary cyst, intradural extramedullary cyst, extradural intraspinal hydatid cyst, hydatid disease of the vertebrae, and paravertebral involvement.78
Neurocysticercosis is worldwide the most common parasitic infection affecting the central nervous system. Spinal neurocysticercosis is unusual even in endemic regions. Infection occurs as a result of ingestion of the eggs of the pork tapeworm, Taenia soleum. The larvae are released from the eggs in the stomach after ingestion. The larvae then penetrate the intestinal mucosa, gain access to the bloodstream, and central nervous system involvement may then occur. Spinal neurocysticercosis can occur in either the subarachnoid space or the parenchyma of the cord.79 Extradural and bony involvement may also occur but are extremely rare.32,80
Diagnosis
The most common presenting symptom of spinal epidural abscess is back pain, which nearly always occurs, followed by fevers, which occur about two thirds of the time. Cervical epidural abscess may be present with neck pain, fever, and some degree of neurological dysfunction. Radiculopathy may also be seen. Fever, defined as temperature >101°F, is a presenting sign ~50% of the time and is clearly not required for diagnosis. Neurological dysfunction including weakness, sensory loss, and bowel or bladder dysfunction may also be seen.81
The diagnosis of pyogenic spondylodiskitis is often delayed due to the presentation of the patient with nonspecific signs and symptoms. Additionally, given the relative rarity of these conditions, diagnostic delays of weeks to months are quite common.52 Most commonly patients present with back pain, which occurs in 60% to 95% of patients.82 Other symptoms include muscle weakness (33% to 68% of patients), difficulties with ambulation (55%), sensory disturbance (49%), fevers (43%), and sphincteric disturbance (25%).48,82,83 On examination, patients may have a limited range of motion, severe paraspinal muscle spasm, and tenderness over the infected level.46 Pyogenic vertebral osteomyelitis should also be strongly considered in any patients with pleural effusion of undetermined cause, especially in the presence of back pain.84
Patients with intramedullary spinal cord abscess most commonly present with neurological deficits, followed by pain and fever. Patients with an acute intramedullary abscess may present with a clinical picture similar to transverse myelitis, whereas those with a more subacute abscess may present with deficits similar to an expanding intramedullary spinal cord tumor.55
Blood cultures are positive in one half to two thirds of cases of epidural abscess. Blood and abscess cultures are nearly 100% concordant when both are positive and thus are very helpful in focusing antibiotic therapy.19 Laboratory studies useful in the diagnosis include complete blood count with differential, erythrocyte sedimentation rate (ESR), and c-reactive protein (CRP). Leukocytosis with a moderate elevation in white blood count (WBC) >15,000/mm3 often accompanies spinal epidural abscess but a normal WBC is not uncommon. ESR is consistently elevated (95%) in the presence of epidural abscess.85 Elevation greater than 30 mm/h is common even without fever or leukocytosis.86 Elevations greater than 100 mm/h in a patient with neck pain is highly suggestive of epidural infection.87 CRP is also often elevated. Both ESR and CRP can also be used to follow a response to treatment.
Laboratory studies are also useful in the diagnosis and management of pyogenic vertebral osteomyelitis. These include an elevated erythrocyte sedimentation rate (>20 mm/h as found in more than 95% of cases), and an elevated CRP may be found in nearly all cases.48,82,83 Nevertheless, normally these markers may rise after an invasive procedure where there is no infection. Most often ESR will peak between postoperative days 4 and 6 and will typically normalize within 14 days. The CRP typically normalizes by postoperative day 6.45
Blood cultures are also useful in the laboratory workup of osteomyelitis. They may be positive in 50% to 75% of cases.47,82 These should be drawn in an attempt to isolate the infected organism. Some organisms may be difficult to culture, and a more rapid diagnosis may be obtained by techniques such as polymerase chain reaction (PCR). Although a diagnosis of a vertebral osteomyelitis may be suspected based on examination and imaging, the actual diagnosis should be made using definitive tissue studies, such as blood culture, PCR, or a vertebral body biopsy.52 Though a urinalysis may be useful in suggesting a source of infection, certainly other sources should be sought because a biopsy may actually identify infection related to a different organism.46,53
For epidural abscess, magnetic resonance imaging (MRI) with contrast is the diagnostic imaging modality of choice.88 Typical MRI characteristics of spinal epidural abscess are a heterogeneously enhancing epidural collection that is iso-/hypointense on T1-weighted images and hyperintense on T2-weighted images19 (Fig. 24-1). Liquid pus in a spinal epidural abscess typically has low signal intensity on T1-weighted imaging, whereas granulation tissue typically has a rim of enhancement after gadolinium injection.89 In cases of a nontuberculosis bacterial abscess, there is often associated spondylodiskitis where hypointense signal changes are seen in the disk and adjacent vertebral bodies on T1-weighted images and a high signal are seen on T2-weighted images. There is usually marked enhancement of the affected vertebral body. In cases attributable to tuberculosis, both epidural involvement and spondylodiskitis have been described with an isointense or hypointense appearance on T1-weighted MRI and a hyperintense appearance on T2-weighted imaging. Additionally, large paraspinal masses are often seen with similar MRI characteristics.90 In patients in whom an MRI cannot be obtained, a computed tomographic (CT) myelogram can demonstrate the lesion well but carries with it the added risks of myelography, including the risk of seeding infection into the subarachnoid space if concomitant lumbar epidural abscess exists. MRI with contrast and CT myelogram have been shown to have equivalent sensitivities (91% to 92%) in detecting epidural abscess.19
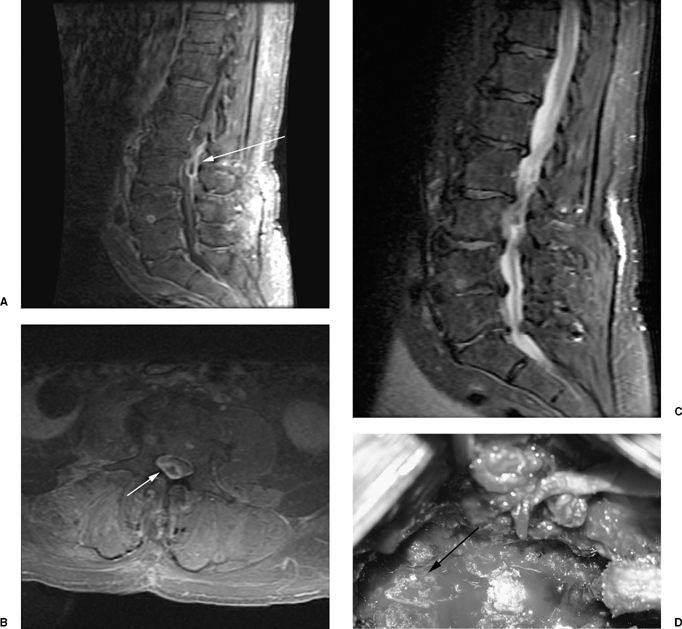
Figure 24-1 Spinal epidural abscess. (A) T1 sagittal image post contrast administration demonstrating a lumbar dorsal epidural abscess at L2-L3 (arrow). Note the rim enhancement with a central hypointense area, suggestive of granulation tissue. (B) On T2-weighted imaging the lesion is hyperintense to the neural elements but less intense than cerebrospinal fluid. (C) Axial T1 image post contrast administration demonstrating significant thecal sac compression secondary to the posteriorly situated mass (arrow). The patient, who presented with back pain, fever, lower extremity weakness, and bladder dysfunction, was treated with L2-L3 laminectomy and evacuation of the abscess. (D) At surgery the patient was noted to have minimal pus but thick granulation tissue compressing the dura (arrow).
For vertebral osteomyelitis, plain radiographs may show changes in the vertebral body or the disk by week 4 of infection; these are often not seen until 8 weeks of infection.91,92 Radiographic findings in osteomyelitis include disk space narrowing, parting of the end plates, and evidence of soft-tissue swelling. By weeks 8 to 12, osteosclerosis may be seen (Fig. 24-2).92 More sensitive are radionuclide bone scans with technetium-99 methylene diphospate. These, however, will not be positive for any bone-forming process and are thus not specific for inflammatory disorders.91,92 More specific for inflammatory processes are bone scans with gallium 67 or indium 3. A combination of gallium and technetium may have greater sensitivity and specificity than either scan alone.90 Nevertheless, given the lack of sensitivity and specificity overall of plain radiographs, other modalities, including a CT scan and an MRI scan, have been used as the hallmark for radiological diagnosis.50,91,92 MRI is considered the imaging method of choice because it has a sensitivity of greater than 80% and specificity between 53% and 94%.50,91 MRI is particularly useful because it demonstrates suspected lesions as decreased signal on T1-weighted imaging and hyperintensity on T2-weighted imaging.91 The administration of gadolinium may result in enhancement of infection on T1-weighted imaging.50,91,93 As discussed later on, postoperative MRI changes may be as difficult to assess, especially in the setting of suspected vertebral osteomyelitis. MRI changes may be normal or they may be indicative of infection, especially if there is evidence of changes involving both the nucleus pulposus and the adjoining vertebral marrow, or changes in the consistency of the disk space when the disk was not removed surgically.51
For intramedullary spinal cord abscess, plain films may reveal associated vertebral osteomyelitis. Although a myelogram may demonstrate a block or a widened spinal cord, MRI has become the imaging modality of choice for intramedullary abscesses. MRI typically shows a low-intensity lesion on T1-weighted imaging and high signal on T2-weighted imaging. Early T1 imaging with contrast reveals a poorly defined area of marginal enhancement, whereas follow-up imaging may show well-defined enhancement of a spinal cord lesion with a central hypointensity.54,94
Tuberculosis-related spinal infections tend to be more indolent and of more gradual onset than pyogenic osteomyelitis. More common symptoms include spinal pain, local tenderness, and night sweats. With cervical involvement, dysphagia, hoarseness, and cervical lymphadenopa-thy may occur.4 Due to its slow and insidious progression, nonspecific presentation, and the mildness of its associated back pain, considerable delay in diagnosis may occur. Significant bone and disk destruction may occur prior to diagnosis.95
On examination, patients with spinal tuberculosis may have spinal tenderness with spasm in the region of the pain. Range of motion testing may elicit severe pain. With advanced disease, the patient may have a Pott’s kyphosis in the thoracic or lumbar spine with collapse of the involved vertebral body resulting in sharp angulation and subsequent prominence of the spinous process at that level. Some patients may demonstrate a psoas sign on exam due to an anterior abscess tracking into the psoas muscle. Patients with a psoas sign lie flat with their hips flexed; when their hips are extended they experience severe pain.95
Radiological findings usually support the diagnosis earlier than laboratory testing. Plain radiographs may reveal vertebral body collapse. Occasionally a lytic lesion may be seen within an involved vertebral body or within the posterior elements.61 Plain radiographs may also reveal osteoporosis, a gibbus deformity, and scoliosis.4 Most frequently, however, plain films are within normal limits.61 CT examination frequently shows destruction at the level of the vertebral end plates, paravertebral abscesses that may have calcifications, and epidural collections. The cortical definition of the affected vertebral body is frequently lost; this is in distinction from pyogenic vertebral osteomyelitis where their cortical borders tend to be preserved. Rim enhancement of a paraspinal mass with calcifications within the mass is highly suggestive of spinal tuberculosis.4 MRI is considered the imaging modality of choice for spinal tuberculosis (Fig. 24-3). MRI may reveal sparing of the disk space with involvement of the vertebral body on either side of the disk, an unusual finding if malignancy is a consideration.95 Additionally, an epidural mass with a bilobed configuration may be seen. MRI is also very useful for demonstrating bony involvement with infection, paraspinal masses, and fistula formation.4 MRI can also demonstrate enhancing intradural and/or intramedullary tuberculomas.61
The diagnosis of spinal tuberculosis should be confirmed by biopsy. Acid-fast bacillus organisms may or may not be seen on stain and may take 6 to 8 weeks to grow; PCR testing is much more rapid. Nevertheless, it is only approved for pulmonary tuberculosis. Additional supportive evidence may come from chest radiographs, purified protein derivative, and sputum/urine culture.94 These tests support the diagnosis but are not definitive when compared with biopsy and culture of the spinal involvement. Although ESR may be elevated and may be useful for following treatment, it is often within normal limits.4,61

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








