Spinal Tumors
David Cachia
Claudio E. Tatsui
Mark R. Gilbert
INTRODUCTION
Tumors of the spinal cord or nerve roots are similar to intracranial tumors in cellular type. They may arise from the parenchyma of the cord, nerve roots, meninges, intraspinal blood vessels, sympathetic nerves, or vertebrae. Metastases may arise from remote tumors.
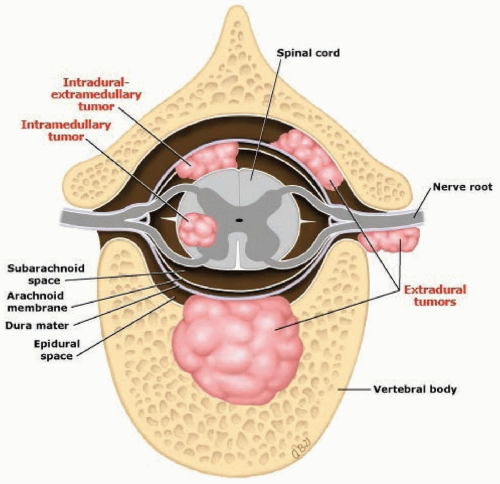
Spinal tumors are divided by location into three groups: intramedullary, extramedullary intradural, or extradural (or epidural) (Fig. 103.1). Occasionally, an extradural tumor extends through an intervertebral foramen to be partially within and partially outside the spinal canal (e.g., dumbbell or hourglass tumors; Fig. 103.2).
EPIDEMIOLOGY
Spinal cord tumors are much less prevalent than intracranial tumors, in a ratio of 1:4, but this varies by histology. The intracranial-to-spinal ratio of astrocytoma is 10:1, and the ratio for ependymomas varies from 3:1 to 20:1, although spinal tumors are the most prevalent location of ependymoma in adults. Men and women are affected equally often, except that meningiomas are more common in women and ependymomas are more common in men. Spinal tumors occur predominantly in young or middle-aged adults and are less common in childhood or after age 60 years.
Spinal tumors appear most often in the thoracic region, but if the relative lengths of the divisions of the spinal cord are considered, the distribution is comparatively equal.
PATHOBIOLOGY
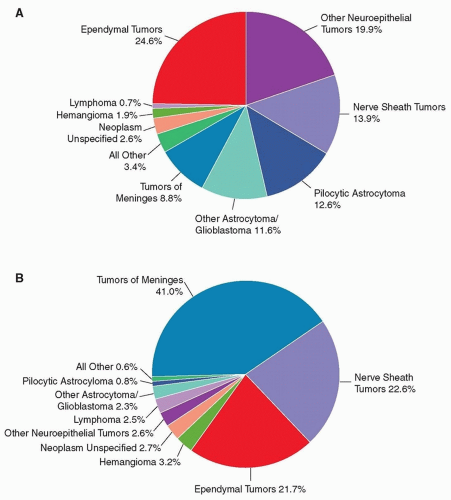
The histologic characteristics of primary and secondary tumors are similar to those of intracranial tumors. An analyses of data from the Surveillance, Epidemiology, and End Results (SEER) and National Program of Cancer Registries that included 11,712 cases of primary spinal tumors identified over a 4-year period showed that of these, 78% were benign and 22% malignant. Histologically, the three most common tumors were meningioma, nerve sheath tumors, and ependymoma.
The most recent Central Brain Tumor Registry of the United States (CBTRUS) data on primary brain and CNS tumors showed that in the age group 0 to 19 years, the most common histology were ependymal tumors followed by other neuroepithelial tumors, whereas in the 20 years and older age group, tumors of the meninges predominate (Fig. 103.3).
The most frequent extradural or epidural tumors are metastasis with the most common primary sites of metastatic tumors to the spine being, in order of frequency—lung, breast, and prostate. Other common metastatic malignancies include tumors of the gastrointestinal tract, lymphomas, melanomas, kidney, sarcomas, thyroid, multiple myeloma, and plasmocytomas.
CLINICAL MANIFESTATIONS
Extramedullary tumors cause symptoms by compressing nerve roots or spinal cord or by occluding the spinal blood vessels resulting in regional ischemia and infarct. The symptoms of intramedullary tumors result from direct interference with the intrinsic structures of the spinal cord from mass effect, edema, or development of syringomyelia. Descriptions of special syndromes follow.
EXTRAMEDULLARY TUMORS
These tumors may be either intradural or extradural (epidural). They usually involve a few spinal cord levels and cause focal signs by compressing nerve roots, particularly the dorsal roots. Extramedullary tumors may ultimately affect the spinal cord, potentially progressing to complete loss of function below the level of the lesion. The first symptoms are typically focal pain and paresthesias, arising from pressure on the dorsal nerve roots. This symptom pattern is soon followed by sensory loss, weakness, and muscular wasting in the distribution of the affected roots. Compression of the spinal cord first interrupts the functions of the pathways that lie at the periphery of the spinal cord. The early signs of cord compression usually include those referable to upper motor neurons such as spastic weakness below the lesion, overactive tendon reflexes, Babinski signs; impairment of cutaneous and proprioceptive sensation below the lesion; impaired control of the bladder and, less often, the rectum; and loss of superficial abdominal reflexes. Occasionally, symptoms may be those of lower motor neurons, such as underactive or absent reflexes with flaccid weakness, especially if the compression occurs abruptly as in spinal “shock” from trauma. If untreated, this syndrome may lead to signs and symptoms of complete transection of spinal cord, with wasting and atrophy of muscles at the level of the root lesion and, below the lesion, paraplegia or quadriplegia. The earliest and only sign can be pain, and the absence of other signs or symptoms may give the misleading impression that the cord is not compressed.
The severity and distribution of weakness and sensory loss varies, depending in part on the location of the tumor in relation to the anterior, lateral, or posterior portion of the spinal cord. Eccentrically placed tumors may cause a typical Brown-Séquard syndrome, namely, ipsilateral signs of posterior column and pyramidal tract dysfunction, with contralateral loss of pain and temperature due to involvement of the lateral spinothalamic tract. Usually, however, because of the external compression, the Brown-Séquard features are incomplete.
Spinal vessels may be occluded by extradural tumors, particularly metastatic carcinoma, lymphoma, or abscess. When the arteries destined for the spinal cord are occluded, the resulting myelomalacia causes signs and symptoms similar to those of a severe intradural process leading to necrosis of the spinal cord. Occlusion of major components of the anterior spinal artery, however, results in segmental lower motor neuron signs at the appropriate level, bilateral loss of pain and temperature sensation, and upper motor neuron signs below the lesion with preservation of dorsal column function (proprioception, discriminative tactile function, and vibration).
Extradural (Epidural) Tumors
Extradural lesions constitute the most frequent group of spinal tumors. Metastatic spinal disease accounts for 95% of those lesions, whereas primary bone tumors account for the remaining 5% of spinal lesions. In general, benign lesions within the vertebral bones are usually asymptomatic and found incidentally, whereas malignant
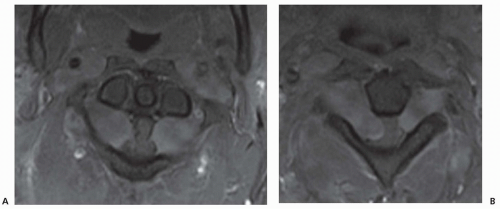
vertebral tumors cause back pain, mechanical instability, pathologic fractures, and sometimes neurologic symptoms due to spinal cord compression. In addition to metastatic cancers, other malignant extradural tumors include multiple myeloma (Fig. 103.4), chordoma, Ewing sarcoma, and chondrosarcoma.
vertebral tumors cause back pain, mechanical instability, pathologic fractures, and sometimes neurologic symptoms due to spinal cord compression. In addition to metastatic cancers, other malignant extradural tumors include multiple myeloma (Fig. 103.4), chordoma, Ewing sarcoma, and chondrosarcoma.
The most frequent benign bone lesions are hemangioma, enostosis, osteoid osteoma-osteoblastoma, aneurismal bone cyst, eosinophilic granuloma (histiocytosis), giant cell tumor, and osteochondroma. Although considered benign, these lesions can be locally aggressive associated with pain, spinal deformity, pathologic fractures, and neural elements compression. Spinal cord metastases will be discussed in greater detail in the following section.
Epidural Spinal Cord Metastasis
Epidural spinal metastasis may be considered a disorder of the vertebral column; the neurologic consequences result from extension of tumor into the spinal canal. Although currently estimated to occur in about 5% to 10% of all cancer patients, as the survival of patients with systemic cancers improves, the incidence of epidural spinal cord compression has increased. Most studies have demonstrated that treatment of cord compression does not prolong survival, but prompt treatment may have an important palliative role, alleviating pain and preventing neurologic disability.
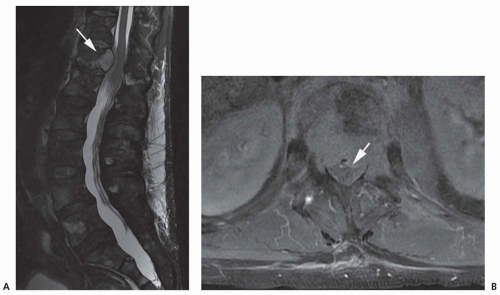
Signs and symptoms of epidural spinal cord compression can be overlooked in a patient with disseminated cancer because of the presence of diffuse pain and asthenia. However, persistent neck and back pain which typically gets worse at night or at rest should prompt an investigation, not waiting for neurologic dysfunction to ensue. Limb weakness or paresthesias in the distribution of a nerve root and bowel or bladder dysfunction make this a neurooncologic emergency that commands prompt evaluation and treatment. Rarely, aside from pain, the only manifestation of cord compression may be a gait disorder, often due to sensory ataxia, without overt evidence of weakness or cutaneous sensory loss. In this situation, it may even be difficult to demonstrate impaired proprioception. The ataxia may be caused by compression of spinocerebellar pathways. The primary malignancy in more than 50% of cases of epidural cord compression is lung (Fig. 103.5) or breast cancer. Overall, more than 80% of cases arise from primary tumors in lung, breast, prostate, gastrointestinal system, melanoma, or lymphoma.
The mechanism of spread of these tumors to the epidural space includes a direct extension from a paravertebral focus through a nerve root foramen; hematogenous metastasis to the vertebrae with extension from bone into the epidural space; or retrograde spread along the venous plexus of Batson. Hematogenous spread to bone is the most common form, and computed tomography (CT) typically shows lytic
or blastic changes in the vertebral bodies in 85% of those patients. Osteoblastic changes are common with prostate carcinoma and are occasionally seen with breast cancer, whereas osteolytic changes are typically seen in multiple myeloma. CT and magnetic resonance imaging (MRI) are sensitive techniques for the detection of spinal osseous metastases. Importantly, involvement of paraspinal lymph nodes with spread to the spinal canal is common with lymphoma. In this situation, the vertebral bone may be normal on imaging studies and use of screening spinal x-rays will be misleading.
or blastic changes in the vertebral bodies in 85% of those patients. Osteoblastic changes are common with prostate carcinoma and are occasionally seen with breast cancer, whereas osteolytic changes are typically seen in multiple myeloma. CT and magnetic resonance imaging (MRI) are sensitive techniques for the detection of spinal osseous metastases. Importantly, involvement of paraspinal lymph nodes with spread to the spinal canal is common with lymphoma. In this situation, the vertebral bone may be normal on imaging studies and use of screening spinal x-rays will be misleading.
Intradural, Extramedullary Tumors
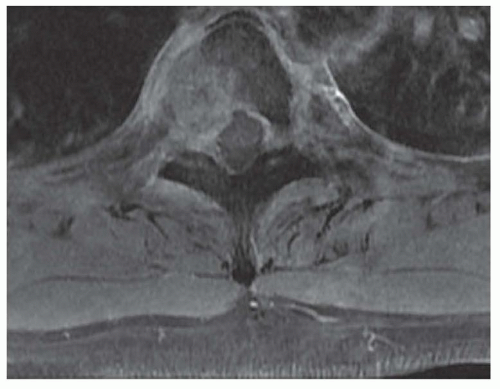
Neurofibromas, schwannomas, and meningiomas are the most commonly occurring primary intradural tumors of the spinal cord. On MRI with gadolinium, the lesions enhance brightly. Meningiomas may be identified by the presence of a dural tail, where the tumor attaches to the dura (Figs. 103.6 and 103.7). Symptoms may occur slowly and some may be asymptomatic despite large size, presumably because of slow growth allowing the spinal cord an opportunity to adapt to the mass effect.
Leptomeningeal metastasis and drop metastases of intracranial tumors also involve the intradural space, but typically, they appear as small nodules attached to the surface of the cord or cauda equina nerve roots (Fig. 103.8), although many (approximately 70%) or not visible on imaging of brain or spine and are detected only by cerebrospinal fluid (CSF) analyses.
INTRAMEDULLARY TUMORS
Primary Intramedullary Tumors
The most common intramedullary tumors are ependymomas and astrocytomas. A diagnosis of von Hippel-Lindau syndrome, an autosomal dominant disorder, should be considered when a spinal hemangioblastoma is present (most commonly involving the thoracic cord) because this association occurs in one-third of the cases. However, rarely, hemangioblastoma can also occur in the intradural extramedullary and extradural locations. Although a single lesion is the most common presentation, multiple lesions occur in one-fifth of cases.
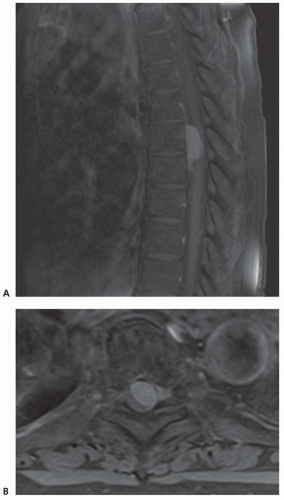
Primary intramedullary tumors usually extend over many segments, causing dilatation of the spinal cord and sometimes causing syringomyelia, which can involve the whole length of the spinal cord. For this reason, the signs and symptoms of intramedullary tumors are more variable than those of extramedullary tumors (Figs. 103.9 and 103.10).
If the tumor is restricted to one or two segments, the clinical presentation can be similar to that of an extramedullary tumor. Pain may be an early manifestation if the dorsal root entry zone is affected. Compression of the crossing pain fibers in the central
cord may cause loss of pain and temperature only in the affected segments. As the tumor spreads peripherally, the spinothalamic tracts may be affected; in the thoracic and cervical areas, pain and temperature fibers from the sacral area lie near the external surface of the cord and may be spared (e.g., sacral sparing). Involvement of the central gray matter destroys the anterior horn cells, with local weakness and atrophy resulting. However, pyramidal fibers may be spared. The clinical picture may be identical to that of syringomyelia with a “suspended” sensory level.
cord may cause loss of pain and temperature only in the affected segments. As the tumor spreads peripherally, the spinothalamic tracts may be affected; in the thoracic and cervical areas, pain and temperature fibers from the sacral area lie near the external surface of the cord and may be spared (e.g., sacral sparing). Involvement of the central gray matter destroys the anterior horn cells, with local weakness and atrophy resulting. However, pyramidal fibers may be spared. The clinical picture may be identical to that of syringomyelia with a “suspended” sensory level.
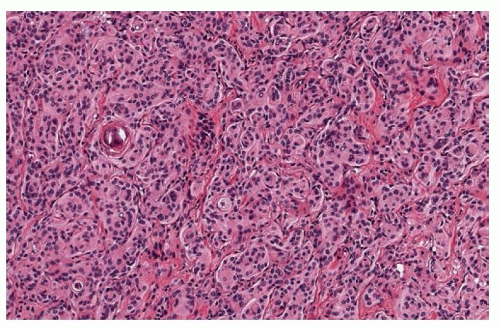 FIGURE 103.7 Meningothelial meningioma of the spinal cord. The classic variant of meningioma is composed of lobules of meningothelial cells separated by fine collagen fibers. The intercellular borders are ill-defined characteristic of a syncytial pattern. Nuclear clearing and whorl formation are frequent. Calcifications (psammoma bodies) might be present. (Courtesy of Dr. Adriana Olar, Department of Pathology, MD Anderson Cancer Center.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|