TABLE 94.1 Disorders Causing Muscle Stiffness and Hyperexcitability | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||
cancer. The disorder is extremely rare in children (eight cases identified older than 29 years at Mayo Clinic and 12 other case reports).
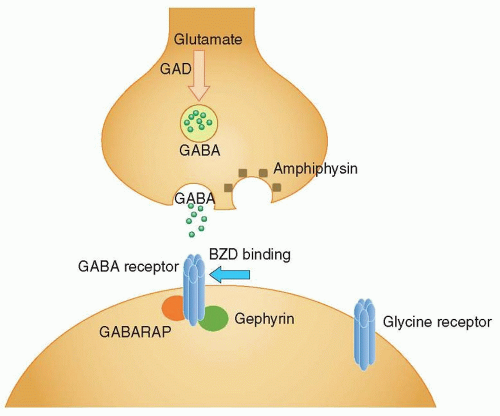
cerebellar ataxia, PERM, and Batten disease), and low titers are associated with other autoimmune diseases (up to 22% of persons with type 1 diabetes mellitus). Other autoantibodies present in SPS include anti-GABARAP in 65% of SPS cases, anti-GlyRα1 antibodies in up to 10% of cases, antiamphiphysin in up to 5% of paraneoplastic cases, and antigephyrin (found in one case of paraneoplastic SPS).
TABLE 94.2 Defining Characteristics of the Stiff Person Syndrome | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree