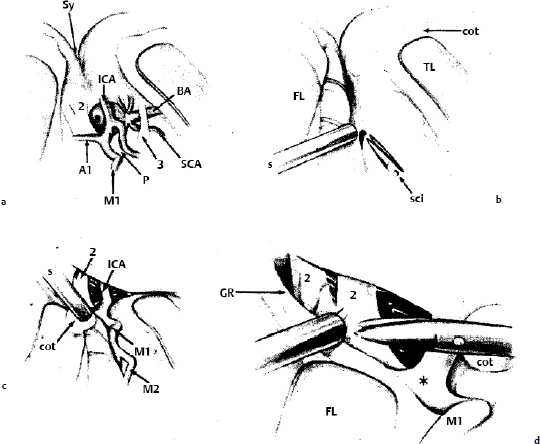
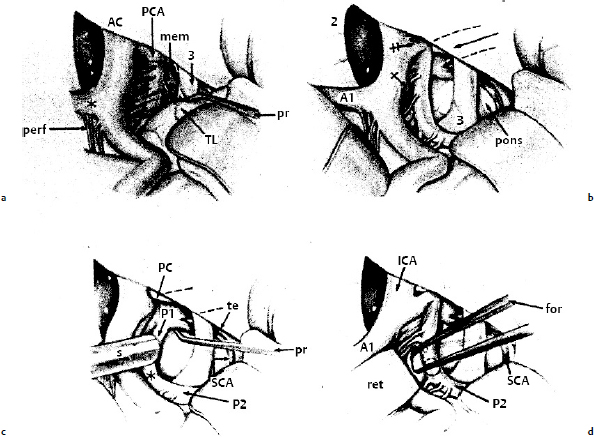
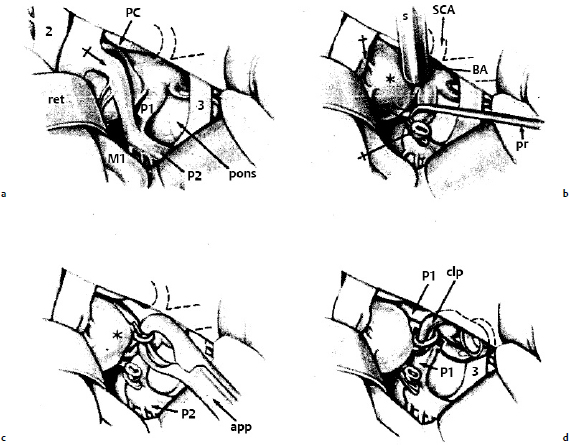
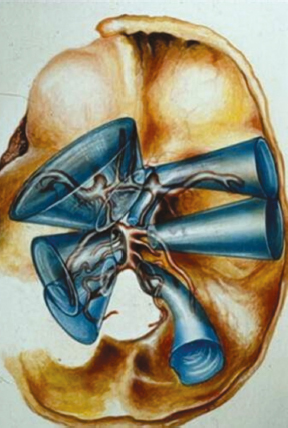
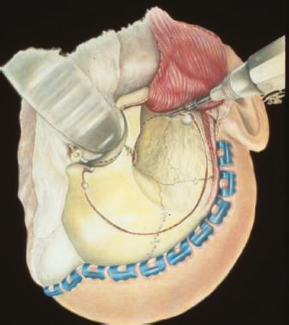
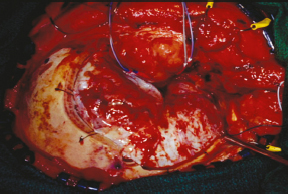
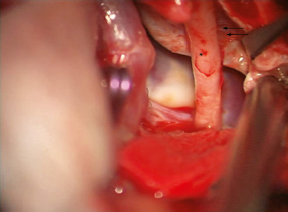
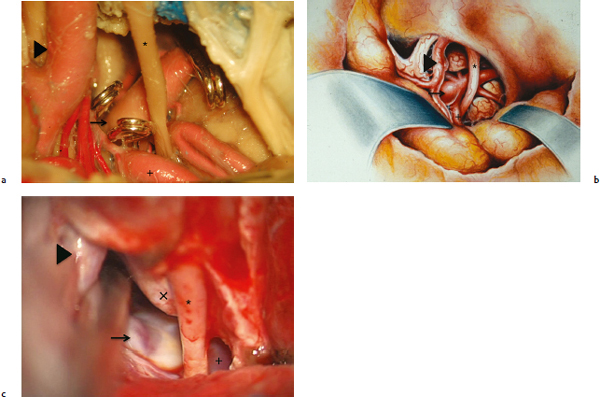
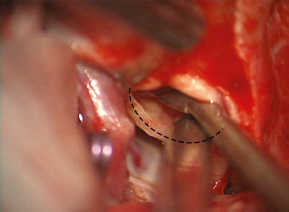
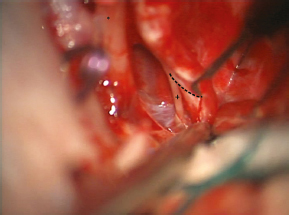
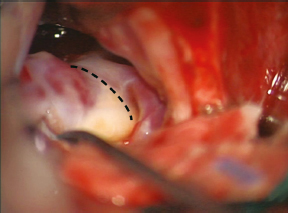
Chapter 16 Case A 45-year-old man who smokes cigarettes presents with subarachnoid hemorrhage of Hunt and Hess grade I and Fisher grade II. A left vertebral artery angiogram and a three-dimensional computed tomography angiography reconstruction show a broad-based basilar tip aneurysm. Participants The Pterional Approach to an Aneurysm at the Basilar Bifurcation: John L. Fox The Cranio-orbital Zygomatic (COZ) Approach to Basilar Apex Aneurysms: Kaith K. Almefty and T. C. Origitano The Transcavernous Approach to Basilar Aneurysms: Ali F. Krisht The Pretemporal Approach to Basilar Aneurysms: Feres Chaddad, José Maria de Campos Filho, and Evandro de Oliveira Moderators: Surgical Approaches to Basilar Apex Aneurysms: Duke Samson and Christopher S. Eddleman Over the past few years, the pterional, or frontolateral, approach to the interpeduncular cistern has gained increasing acceptance.1–6 To visualize any targeted lesion in this cistern between the upper clivus and the midbrain, the surgeon must open a pathway between the sphenoid wing and the base of the sylvian fissure. Failure to drill the sphenoid wing and insufficient opening of the sylvian fissure under good magnification have been common causes of a surgeon’s disappointment in using the pterional approach. Figure 16.1a illustrates the relationship of the aneurysm to cerebral structures as seen through a right pterional approach. Figure 16.1b,c shows the opening of the sylvian fissure. Figure 16.1d emphasizes the lysis of the arachnoid and adhesions between the optic nerve and the base of the frontal lobe. Fig. 16.1a–d (a) The projected relationship of an aneurysm at the basilar bifurcation to arteries and nerves as seen in the right frontotemporal or pterional approach after the sylvian fissure (Sy) is opened. Note the right A1 artery crossing the chiasm behind the optic nerve (2); the internal carotid artery (ICA) continuing toward the surgeon as the M1 artery; the right oculomotor nerve (3) arising from the midbrain and flanked by the posterior cerebral artery rostrally and the superior cerebellar artery (SCA) caudally (seen on the left side also); the termination of the basilar artery (BA); and the junction (p) of the right posterior communicating P1 and P2 arteries. (b) The arachnoid in the sylvian fissure is incised with microscissors (sci). The surgeon holds the suction tube(s) in the left hand. Self-retaining retractors support and separate the frontal lobe (FL) and temporal lobe (TL). cot, cotton ball. (c) The sylvian fissure has been opened widely, exposing M1 and M2 and the internal carotid artery (ICA), as well as the optic nerve (2). The tip of the suction tube(s) rests on a small dental cotton ball (cot). (d) The retractor is used to elevate the right frontal lobe (FL) and its gyrus rectus (GR) off the optic nerves (2) and chiasm. Arachnoid adhesions between the chiasm and frontal lobe are severed. The middle cerebral artery (M1) and bifurcation of the internal carotid artery (*) are in view. (From Fox JL. Microsurgical exposure of vertebrobasilar aneurysms. In: Rand RW, ed. Microneurosurgery, 3rd ed. St. Louis: CV Mosby, 1985:589–599. Reprinted by permission.) In Fig. 16.2, we see the pathway taken caudally. The wide separation of the right frontal and temporal lobes with visualization of the middle cerebral artery is evident. The exposure is developed between the internal carotid artery and the oculomotor nerve; the posterior communicating artery is followed (Fig. 16.2a,b). Occasionally, the exposure is between the optic nerve and the internal carotid artery (rare in my experience). The rostral pons, the superior cerebellar artery, the origin of the oculomotor nerve, and the junction of the posterior communicating artery with the P1 and P2 portions of the posterior cerebral artery (PCA) are evident (Fig. 16.2c,d). At times, the posterior clinoid process is in the visual field. In such uncommon cases, I use a small high-speed diamond drill to remove this projection. Figure 16.3a shows the aneurysm at the tip of the basilar artery coming into view between the retracted right internal carotid artery and the oculomotor nerve. Often, the posterior communicating artery must be severed between small malleable clips (avoiding perforators) to gain an adequate view of the aneurysm (Fig. 16.3b). After the aneurysm is separated from the posterior thalamic perforators, the neck is clipped (Fig. 16.3c,d). A large aneurysm, such as that seen in the patient under discussion, often requires a long clip to be placed across the equator of the dome to collapse the aneurysm before clipping the neck. Otherwise, the clip on the neck will slip and occlude the P1 arteries. Fig. 16.3a–d (a) A narrow retractor (ret) is used to displace the internal carotid bifurcation and M1. The crossed arrow points to the posterior communicating artery lying lateral to the dome of the aneurysm. The optic (2) and oculomotor (3) nerves are seen. The posterior clinoid process (PC) hides part of the left P1 artery. The right P1 and P2 arteries and the rostral pons are seen. (b) The posterior communicating artery (single-crossed arrows) has been clipped with small, malleable, tantalum clips and severed to better expose the aneurysm (*). The suction tube(s) hides the junction of the left P1 and the aneurysm. The tip of the basilar artery (BA) is seen. The left superior cerebellar artery (SCA) is hidden. A probe (pr) is used to retract the right P1 artery to expose the posterior thalamoperforators. (c) A Yasargil clip straddles the neck of the aneurysm (*) before closure. The clip is in its applicator (app). The right P2 artery is seen. (d) The clip (clp) has been closed. Both P1 arteries and their perforators are preserved. The shank of the clip touches the oculomotor nerve (3). (From Fox JL. Microsurgical exposure of vertebrobasilar aneurysms. In: Rand RW, ed. Microneurosurgery, 3rd ed. St. Louis: CV Mosby, 1985: 589–599. Reprinted by permission.) Samson and colleagues7 and Wright and Wilson8 have emphasized the importance of appreciating the relationship of the posterior clinoid process to the neck of the aneurysm on the lateral arteriogram. They concluded that the fronto-lateral approach is too difficult if the neck of the aneurysm lies below the level of the posterior clinoid process. With wide opening of the sylvian fissure, however, and excellent brain relaxation, I believe it is still usually possible to deal with these low-lying basilar tip aneurysms. Yasargil and colleagues6 preferred the frontolateral to the subtemporal route for the following reasons: • There is less retraction pressure on the temporal lobe. • The anatomy of the interpeduncular cistern is better seen (both P1 arteries and perforators) with a more frontal view of the aneurysm. • The oculomotor and trochlear nerves are less disturbed. The disadvantages of the frontolateral route may include the following: • The internal carotid or M1 arteries must often be retracted (this is dangerous if the patient has atherosclerosis or if blood pressure drops very low). • The posterior communicating or P1 artery must often be ligated and sectioned. • The posterior clinoid process may be in the way of lowlying aneurysms at the basilar bifurcation. • Aneurysms high up in the interpeduncular cistern that project backward are more difficult to visualize. • Perforators between the posterior aspect of the aneurysm and the brain stem may be less easily seen in some cases. • The working space between the internal carotid artery and the oculomotor nerve is confining, requiring expert microtechnique. Some surgeons have used a modified approach that combines the pterional exposure with the subtemporal, usually resulting in posterior retraction of the temporal lobe rather than a true transsylvian exposure.9,10 The supraorbitalpterional approach of Al-Mefty11 provides further low-basal exposure of these lesions. Early in my neurosurgical career, I operated on aneurysms at the basilar bifurcation through the standard sub-temporal approach described by Drake.12 After observing the techniques of Yasargil and colleagues6 (who first used the pterional approach for those aneurysms), I changed to using the pterional approach because many patients had multiple aneurysms that could not all be clipped through the subtemporal approach during the same surgery. As I gained experience, I found myself more comfortable with the pterional approach and now rarely use the subtemporal approach to aneurysms in the interpeduncular fossa. In the patient described in this case, I would use the right pterional approach, operating when the patient is in good condition after the phase of vasospasm has passed. Basilar apex aneurysms are among the most challenging cerebrovascular lesions because of their deep location, proximity to important and delicate neurovascular structures, and the surgeon’s limited visibility and maneuverability. The surgical challenges have been exacerbated in the endovascular era as surgical treatment has often been reserved for the most complex geometrical lesions. The ideal surgical approach to these complex lesions should embody the following fundamental principles: • Provide visualization and control of proximal and distal vasculature. • Allow for the safe dissection of small perforating arteries. • Maximize maneuverability and ergonomics for optimal dissection and clip placement with minimal brain retraction.13 The cranio-orbital zygomatic (COZ) approach achieves these tenets by providing a shorter and wider operative distance, early proximal and distal control, direct entry to the interpeduncular cistern, and multiple angles for viewing and dissecting, as well as minimizing brain retraction. An approach angle that is flat with the middle cranial fossa combined with the short, wide corridor enables the surgeon to place a hand in the middle cranial fossa for improved control (Fig. 16.4). This approach provides clear visualization of the thalamoperforators, the neck and dome of the aneurysm, the anterior circulation, and both PCAs. In addition, the clip can be placed without compromising visualization or control. In this chapter’s presented case, cerebral angiography with three-dimensional reconstruction delineates a broad-based aneurysm at the basilar apex (see the figures with the case presentation), and so this patient is considered high risk for endovascular treatment. We recommend that the patient undergo definitive clipping of the aneurysm through a right-sided COZ approach with removal of the posterior clinoid process and a transcavernous technique. For this approach, the patient’s head is placed in the Mayfield headrest (with all pins placed behind the ears if possible), slightly extended, and turned 30 degrees away from the operative side. A scalp incision is made 1 cm anterior to the tragus and continued behind the hairline to the midline. This incision can be extended toward the contra-lateral temporal line for additional exposure, and should be superficial to the pericranium and temporalis fascia. The subcutaneous flap is dissected sharply from the pericranium, and dissection is carried anteriorly to the prominence of the superior orbital rim. Further dissection in this plane is done posterior to the skin incision. A bicoronal incision is then made in the underlying pericranium, from temporal line to temporal line, based on the supraorbital blood supply. The large vascularized flap is then elevated, and the supraorbital arterial supply is preserved along the bilateral superior temporal lines. The supraorbital nerve should be identified along the medial third of the superior orbital notch. It may exit either through a notch or a true foramen. If through a notch, the nerve can be safely dissected free. If through a foramen, an osteotomy must be done around the foramen and the nerve dissected free with its bony attachment. The periorbita is detached from the superior and lateral walls of the orbit and the scalp flap is reflected anteriorly. Fig. 16.4 Illustration showing the surgical approaches to the cerebral vasculature. The top left cone shows the cranio-orbital zygomatic (COZ) approach. The right top and middle cones show the pterional and subtemporal approaches, respectively. Note the short wide corridor to the basilar apex obtained with the COZ approach compared with the longer, more narrow corridors of the traditional approaches. (From Origitano TC, Anderson DE, Tarassoli Y, Reichman OH, Al-Mefty O. Skull base approaches to complex cerebral aneurysms. Surg Neurol 1993;40:339–346. Reprinted by permission.) To protect the frontotemporal branches of the facial nerve, the fat pad containing these branches is elevated with the superficial and deep layers of temporalis fascia. At a point 1.5 cm posterior to the lateral orbital rim, a 2-cm incision in the superficial and deep temporal fascia is made parallel with the zygomatic arch. In subperiosteal fashion, these layers are reflected with the fat pad and skin flap. The zygomatic arch is also dissected along its length in subperiosteal fashion. It is then sectioned obliquely at the malar eminence and the root of the zygoma. The temporalis muscle is incised posterior to the superficial temporal artery, elevated with subperiosteal dissection, and reflected downward.14 Bur holes are placed at the base of the zygoma and at the keyhole, which should expose both the dura and periorbita. An osteotomy is made on the lateral orbital rim and extended to the keyhole. The next cut extends from the zygomatic bur hole along the base of the temporal fossa to the sphenoid ridge. The sphenoid ridge is then removed with the high-speed drill, and this cut is connected to the keyhole. An osteotomy is then made from the temporal bur hole to the frontal bur hole and extended into the orbital roof. Next, an osteotomy is done from the keyhole through the orbital roof, extending medially. The skull flap can then be elevated, and the remaining portion of the roof and lateral orbit are removed in one piece with additional osteotomies. The first cut is in the roof of the orbit and extends posteriorly along but not into the ethmoid sinuses. The second cut is made at the base of the lateral wall of the orbit along the inferior orbital fissure. These cuts are then connected across the lesser sphenoid wing and the flap is elevated15 (Fig. 16.5). The osteotomies can be tailored to individual aspects of the patient’s anatomy and based on the surgeon’s experience. They can be done as described above, or the orbitozygomatic osteotomy can be taken as a single piece or as two pieces (orbit and zygoma). The medial aspects of the sphenoid wing are removed with the drill, which unroofs the superior orbital fissure. The optic canal is located medial to the superior orbital fissure at the apex of the orbit. It is opened extradurally and the optic strut is drilled, allowing for an extradural removal of the anterior clinoid process (Fig. 16.6). The dura is then opened with a curvilinear incision and reflected anteriorly. The surgeon can gain additional working space by depressing the orbit with anterior dural traction and fixation to further flatten the orbital trajectory.16,17 The sylvian fissure is widely dissected, allowing the temporal lobe to fall laterally and posteriorly. The tethering veins running from the sylvian fissure to the sphenoparietal sinus are dissected and preserved. The lateral and medial carotid cisterns, the lateral wall of the cavernous sinus, and the edge of the tentorial incisura are then exposed. The entrance of the third nerve into the cavernous sinus must be identified and will guide further dissection. Untethering the third nerve and opening the oculomotor foramen provides additional exposure and facilitates safe retraction of the nerve (Fig. 16.7). Dissection is done along the third nerve toward the brainstem, and the origins of the PCAs and superior cerebellar arteries are identified. At this point, proximal control of the distal basilar artery should be established by identifying a “landing zone” for the application of a temporary clip. The posterior communicating artery is dissected from its origin on the carotid to the junction of the PCA. Beneath the posterior communicating artery, the interpeduncular cistern is approached obliquely from an anterior-to-inferior direction, and the posterior communicating artery is followed back to the PCA and the aneurysm. The superior aspect of the aneurysm is further dissected anterior to the third nerve in the interpeduncular cistern (Fig. 16.8). The back wall of the aneurysm and the thalamoperforators may be dissected by working laterally and beneath the third nerve. Fig. 16.5 Illustration of the COZ cuts. Bur holes are drilled in the temporal bone (the keyhole) and the frontal bone. Cuts are made as follows: from the lateral orbital rim to the keyhole, the zygomatic bur hole to the sphenoid ridge, the temporal bur hole to the frontal bur hole, the keyhole through the orbital roof extending medially, and the sphenoid ridge to the keyhole. (From Arnautovic KI, Al-Mefty O, Angtuaco E. A combined microsurgical skull-base and endovascular approach to giant and large paraclinoid aneurysms. Surg Neurol 1998;50:504–520. Reprinted by permission.) Fig. 16.6 Intraoperative photograph of the COZ craniotomy. The temporalis muscle is reflected inferiorly and out of the field of view. The orbital osteotomies have widened the transsylvian corridor. This exposure is typically sufficient for high-lying and normal basilar apex aneurysms; for low-lying aneurysms, additional exposure may be necessary. Skeletonizing and removing the posterior clinoid process may create further anterior and lateral exposure (Fig. 16.9). Exposing the proximal basilar artery for temporary clipping is possible at the level of the fifth nerve; cutting the tentorium behind the fourth nerve facilitates this by allowing for further inferior visualization13,16 (Fig. 16.10). These maneuvers provide a wide exposure of the interpeduncular cistern with multiple viewing angles, allowing the surgeon to view the top of the basilar artery, the posterior communicating artery, and both PCAs. Clips may be applied in a lateral-to-anterolateral arc (Fig. 16.11). If projecting dorsally, the aneurysm may be difficult to clip from this arc and a more lateral trajectory can be obtained by working through the ambient cistern. The COZ approach allows for this with minimal retraction of the temporal lobe.16 Fig. 16.7 The oculomotor foramen is opened, a maneuver that widens the depth of field and allows for safe manipulation of the nerve. Arrows: oculomotor nerve; arrows oculomotor foramen. The COZ approach, as described here and with variations by others,13,14,16,18–20 provides distinct advantages in the clipping of basilar tip aneurysms as compared with the pterional and subtemporal approaches. The lateral sub-temporal approach to basilar apex aneurysms provides the advantage of exposure to the posterior aspect of the aneurysm and to the thalamoperforators, but exposure of the apex and the contralateral P1 is limited. In addition, temporal lobe retraction is necessary and this approach may not be feasible in the setting of subarachnoid hemorrhage and cerebral swelling. The pterional approach provides access to the apex and contralateral P1, but limits the exposure to the back wall of the aneurysm. The trajectory is long, and aneurysms placed both high and low are not well visualized because of the one-directional, envelope-shaped field. The COZ approach provides both superior and posterior access and increases the number of viewing angles, fundamentally providing both the transsylvian and sub-temporal avenues.13,16 The wide exposure of the interpeduncular cistern allows access to the apex of the aneurysm, the carotid artery, and the posterior communicating and PCAs.13,17 Temporary clipping distal or proximal to the superior cerebellar arteries is also possible (Fig. 16.8). The flat working area along the middle cranial fossa exposes the neck and the thalamoperforators. Untethering the third nerve and drilling the posterior clinoid process opens up additional working angles and access to a low-lying bifurcation.16,18 The essential advantage of the skull-base approach is a shorter, wider corridor. This corridor provides the surgeon with greater visualization, maneuverability, control, and ergonomic advantages at the deepest and most delicate points of dissection. The additional working angles ensure safer clipping with better visualization of the thalamoperforators and the contralateral P1.13,15–17 Advancements in endovascular surgery have resulted in fewer basilar tip aneurysms treated through clipping. As a result, the aneurysms approached surgically are often complicated and present unique challenges, such as a large size, wide neck, and difficult projection. The advantages of the COZ approach are most profound in the surgical management of these complicated aneurysms, when both anterior and lateral dissection is necessary for safe and successful clipping. Fig. 16.9 The posterior clinoid is skeletonized and removed to allow additional anterior and lateral exposure.
Surgical Approaches to Basilar Tip Aneurysms

The Pterional Approach to an Aneursym at the Basilar Bifurcation
Surgical Approach
Discussion
The Cranio-orbital Zygomatic (COZ) Approach to Basilar Apex Aneurysms
Case Presentation and Description of the Cranio-orbital Zygomatic Approach
Discussion
< div class='tao-gold-member'>
Surgical Approaches to Basilar Tip Aneurysms
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree