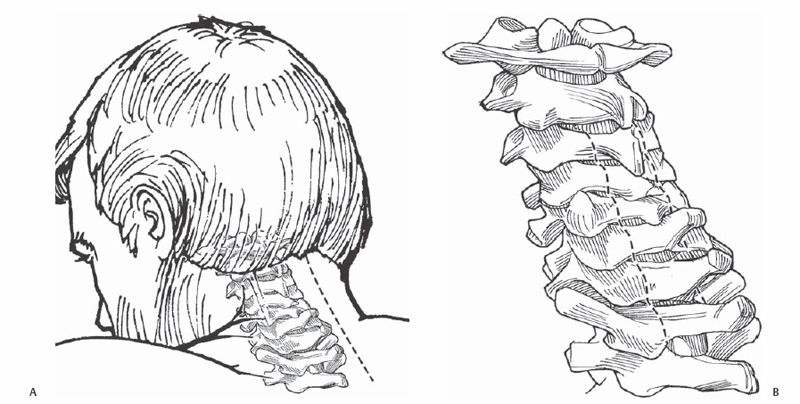
4 Timothy F. Witham and Ziya L. Gokaslan Resection of intradural tumors is performed almost exclusively through a posterior approach. Laminectomies performed rostral and caudal to the level of the lesion are critical to provide adequate exposure for tumor resection. Coronal exposure is also important with wide, but facet-sparing, laminectomies that allow for gentle manipulation of the tumor and spinal cord if necessary. Even ventrally situated tumors can most often be approached in this fashion. A dural opening rostral and caudal to the level of the lesion is critical. The arachnoid should initially be preserved to prevent spinal cord herniation. Opening the dura rostral to the lesion first also helps to prevent herniation of the spinal cord if the arachnoid is not preserved. Techniques to allow for gentle manipulation of the spinal cord include wide laminectomies, a lengthy dural opening, sectioning of the dentate ligaments, and, in some cases, nerve root sectioning. Intradural spinal tumors are classified as extramedullary or intramedullary. In most cases, the extramedullary tumors are benign, and the surgical goal is complete resection. In some cases with lesions such as neurofibromas, complete resection is not possible without complete or partial transection of the nerve root of origin. If the root is one that subserves a critical function (i.e., C5 root) then consideration is given to subtotal resection. The majority of extramedullary tumors may be cured with complete surgical excision. Intramedullary tumors are less likely to be cured by surgery alone. Ependymomas, hemangioblastomas, angiolipomas, and pilocytic tumors are usually amenable to complete resection, whereas malignant astrocytic tumors require subtotal resection or biopsy followed by adjuvant therapy. A contrast-enhancing intradural spinal lesion in a symptomatic patient is usually approached surgically for diagnostic and therapeutic purposes. Symptoms include motor or sensory deficits, sphincter dysfunction, and pain localized to the area of the lesion. Pain that is not mechanical and tends to be exacerbated by recumbency is common with intradural spinal tumors. Transverse myelitis and multiple sclerosis are two disease entities that may be confused with intramedullary spinal cord tumors. Clinical history and imaging can differentiate these diseases from intradural tumors. However, if the clinical picture is not clear, then neurologic workup for demyelinating disease should be initiated. Drop metastases are typically not approached surgically. Elderly patients who are asymptomatic may be initially followed with serial imaging. Tumors with highly aggressive behavior may be considered for biopsy and adjuvant therapy. Perioperative administration of corticosteroids is not supported by scientific evidence. However, many surgeons routinely administer up to 100 mg of Decadron prior to resection of intramedullary tumors and continue high-dose steroids postoperatively. A subsequent slow taper is performed over 2 to 4 weeks. For intradural meningiomas that require dural resection and for intramedullary cases in which spinal cord swelling is a potential issue, a dural patch graft may be necessary. Meticulous dural closure is paramount in the prevention of a cerebrospinal fluid (CSF) fistula or pseudomeningocele. A dural sealant is routinely placed along the suture line as well. Patients are placed in the prone position, and the chest is well padded. A Mayfield cranial clamp is used for cervical and upper thoracic lesions. Perioperative corticosteroids and broad-spectrum antibiotics are routinely administered to all patients. The horseshoe adapter to the Mayfield is avoided to prevent skin breakdown on the face or ocular pressure leading to ocular ischemia that can be observed during prolonged cases in the prone position with this device. For intramedullary spinal cord tumors, the dissection is usually begun at the middle portion of the neoplasm where the lesion is the bulkiest. Dissection in this location is least likely to result in injury to the surrounding neural tissues. For lesions with tumor-associated cysts, laminectomies to provide exposure of the cyst outside the area of the solid tumor component are not necessary. The cyst walls are typically nonneoplastic, and complete tumor resection results in the disappearance of the cyst. Intraoperative monitoring with epidural motor evoked potential (MEPs) leads may be helpful as a way to avoid rather than merely detect irreversible neurologic injury. With experienced electrophysiologists, spinal epidural MEPs are a reliable predictor of postoperative outcome. All patients should be followed with plain radiographs for the development of postlaminectomy kyphosis. Children less than 3 years of age, those with preoperative deformity, and those with preoperative neurologic deficits are at greatest risk. Although there is no scientific evidence to support the use of laminoplasty, this technique is used in all children and in those patients at high risk for the development of postlaminectomy kyphosis. Titanium miniplates can be used to reconstruct and stabilize the lamina. Continuous somatosensory evoked potentials (SSEPs) are monitored in all patients. MEPs are monitored as described above when a good baseline may be followed. Although SSEPs and MEPs are thought to be predictive of postoperative outcome at centers with extensive experience, this finding remains controversial. A standard midline skin incision is fashioned with subsequent subperiosteal dissection of the paraspinal muscles (Fig. 4.1A). Laminectomies or osteoplastic laminotomies are performed one level above and below the superior and inferior poles of the tumor (Fig. 4.1B). Large moist cottonoids are placed along the edges of the paraspinal muscles. Intraoperative ultrasonography is commonly helpful prior to dural opening for intramedullary tumors to determine if the tumor is sufficiently exposed rostrocaudally.
Surgical Removal of Intradural Spinal Cord Tumors
Description
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








