21 The Endonasal Transplanum-Transtuberculum Endoscopic Approach in Pituitary Adenomas
Giorgio Frank, Diego Mazzatenta, Vittorio Sciarretta, Matteo Zoli, Giovanni Farneti, and Ernesto Pasquini
 Introduction
Introduction
In 1987, Weiss,1 using a sublabial microscopic approach, first described the transplanum-transtuberculum approach. Its application using the microsurgical technique was confirmed and popularized by other authors.2–8 The advent of the endoscopic technique helped in reducing the difficulties related to a narrow and deep surgical field and helped to overcome the reduced peripheral vision normally associated with the microscope.9 This made its use more frequent and applicable to a variety of pathologies (craniopharyngiomas, meningiomas, and adenomas).10–13 In theory, the use of the endonasal transplanum-transtuberculum endoscopic approach (ETTEA) in comparison with the standard transsphenoidal approach increases the extent of tumor removal and reduces morbidity with respect to the intracranial approach. In fact, the surgical management of pituitary adenomas rarely requires a transcranial approach (less than 10% in the series of Buchfelder and Kreutzer14 in 2008) and only a few, very select cases are suitable for an ETTEA. The surgical treatment of choice for pituitary adenomas still remains the transsphenoidal approach because it is safe, well tolerated, and effective.12 The transsphenoidal approach facilitates an endocapsular selective adenomectomy, which means selective tumor removal with preservation of the pituitary gland.
The ETTEA induces the pituitary surgeon to take two actions that are contrary to customary practice: the intentional penetration of the subarachnoid space, and an extracapsular dissection of the tumor. The former makes an intraoperative cerebrospinal fluid (CSF) leak unavoidable, and increases the risks of postoperative CSF rhinorrhea and meningitis. However, increased experience in CSF leak repair, using modern techniques that are quite effective (mainly, multilayer plastic repair or a pedicled vascularized flap15,16) has made this condition easier to control, making intraoperative CSF leak an acceptable risk. The postoperative CSF leak rate has dropped to less than 6%.17 An extracapsular dissection of the tumor enables a more radical tumor removal, at the expense of including normal pituitary gland tissue in the excision. Conversely, it is well known that, in pituitary surgery, a partial removal with functional preservation is often preferable to a radical removal with pituitary insufficiency.
The decision to change the management of a pituitary adenoma from a standard transsphenoidal approach to an extended one is not easy, and should be restricted to a few selected cases. Some of these cases would previously have been considered for a transcranial approach.14 It is well accepted that the endonasal extended approach compared with a transcranial approach has the advantage of being a minimally invasive approach, giving direct access to the lesion with no risk of brain manipulation and neurovascular dissection.
The characteristics that make a pituitary adenoma amenable to the ETTEA, as an alternative to the transcranial approach, are the anatomical factors and the midline position of the tumor.11 The anatomical factors favoring an endonasal approach are (1) a well-pneumatized sphenoid sinus; (2) an adequate intercarotid distance; (3) absence of associated vascular anomalies, such as aneurysms; and (4) the absence of vascular encasement by the tumor (Fig. 21.1).
At present, we are convinced that the ETTEA is the procedure of choice for ectopic adrenocorticotropic hormone (ACTH) microadenomas of the pituitary stalk.8
In macroadenomas, such a decision may be facilitated by the presence of pituitary insufficiency and visual disturbances because, under these circumstances, the role of selective adenomectomy is less important with respect to optochiasmatic decompression. We believe that an ETTEA should be considered in adenomas with a midline subfrontal extension, in invasive adenomas growing through the diaphragma sella, and in fibrous tumors.
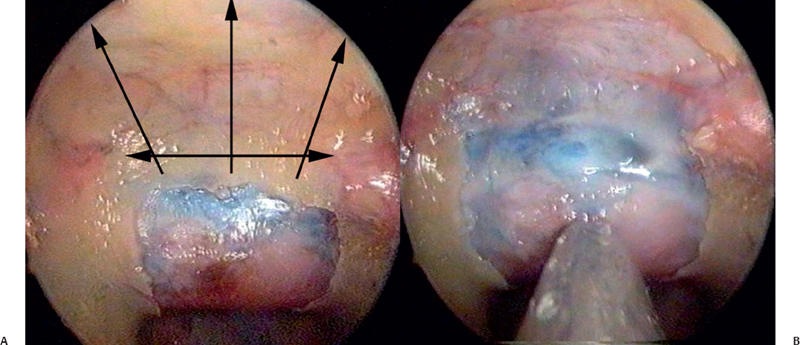
Fig. 21.1 (A,B) Anatomic dissection in an injected specimen. After removal of the sellar bone, the next step is the removal of the bone from the planum following the direction indicated by the arrows in A. The extension of bone removal is related to sphenoidal pneumatization, tumor size, and intercarotid distance.
 Technical Note
Technical Note
We have previously described our technique of ETTEA in several publications.10,18 At present we would emphasize some interesting aspects of our procedure. We place the patient in a semi-sitting position, which we believe offers the advantage of a clearer operative field due to the reduced bleeding and gravity-induced drainage of blood and irrigation fluid away from the operative field. A disadvantage is the increased outflow of CSF and the increased risk of postoperative pneumocephalus. During the crucial phase of the procedure, we place the endoscope in a mechanical holder. This gives the surgeons the ability to carry out a bimanual dissection of the tumor. To increase the maneuverability of the instruments through the narrow surgical channel, we perform a unilateral middle turbinectomy at the beginning and laterally displace the contralateral middle turbinate. In doing so, we avoid also damage to the mucoperiosteum of the middle turbinate, which is needed in the multilayer closure. A wide anterior sphenoidotomy is then performed, and, depending on the size of the sphenoidal sinus, a uni- or bilateral posterior ethmoidectomy sometimes may be necessary to gain adequate control of the floor of the anterior cranial base. Bone removal is tailored to the lesion. It begins in the sellar region and extends to the tuberculum and the planum sphenoidale (Fig. 21.1).
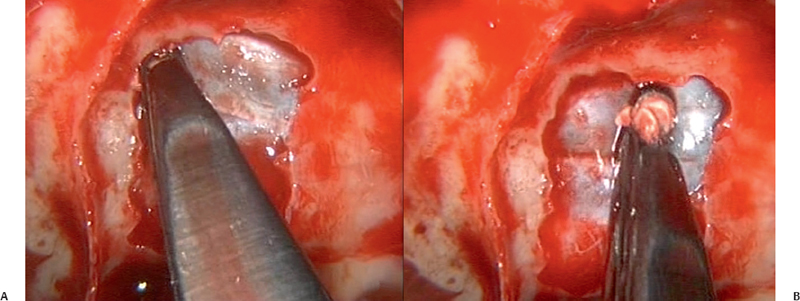
Fig. 21.2 (A,B) Removal of the bone from the planum sphenoidalis is possible using a drill or cutting instrument, such as Kerrison’s rongeurs. When the bone is thin, we prefer to use a cutting instrument to reduce the risk of damage from the heat generated by a high-speed diamond drill.




