7
Trauma to the Temporal Bone
Samuel Thomas von Soemmerring (1755–1830), a German medical student, established the present classification of cranial nerves in 12 numbered pairs two centuries ago based on the different foramina in the base of the skull through which the nerves exit the cranial cavity.1 The first description of traumatic cranial nerve injury appears in the Edwin Smith Papyrus, and describes a patient with a facial droop following head injury.2 This is probably the first account of traumatic facial nerve paralysis recorded.
♦ Applied Anatomy of the Facial Nerve
The two roots of the facial nerve arise from the pons lateral to the recess between the inferior olive and the inferior cerebellar peduncle. The sensory root is called the nervus intermedius and lies close to the eighth cranial nerve until it reaches the internal auditory meatus. Inside the internal auditory canal, the facial nerve is connected to the vestibular nerve by the fibers of Rasmussen. At the lateral fundus of the meatus it pierces the arachnoid and the dura to enter the facial canal superior to the transverse crest, separated from the superior vestibular nerve by Bill’s bar and accompanied by the labyrinthine branch of the anterior inferior cerebellar artery (AICA). This labyrinthine segment runs across the axis of the petrous pyramid to the geniculum and forms the geniculate ganglion and then turns 130 degrees as it becomes the tympanic or horizontal segment. The pyramidal part connects the horizontal and the mastoid segments and gives off the nerve to the stapedius muscle. The nerve now descends to the stylomastoid foramen and gives off the chorda tympani nerve (Fig. 7.1).
The temporal bone is developed from five developmentally and morphologically distinct parts. The cartilaginous petromastoid part develops to preserve the precise orientation of the membranous labyrinth. The mastoid serves as an anatomic door to the petrous pyramid, the base of which arbitrarily corresponds to the suture between the petrous and squamous elements. The apex of the petrous pyramid is blunt and irregularly angled between the posterior border of the greater wing of the sphenoid and the basiocciput bone. The anterior surface partly forms the floor of the middle cranial fossa and is continuous with the cerebral surface of the squamous part adapted to the inferior temporal gyri. Laterally the apex forms the roof of the vestibule and part of the facial canal. Between the arcuate eminence (lodging the superior semicircular canal) and the squamous temporal bone is the tegmen tympani, which forms the roof of the mastoid antrum. The posterior surface of the petrous pyramid is an anterior part of the posterior cranial fossa and is continuous with the internal mastoid surface. The superior border of the petrous bone is grooved by the superior petrosal sinus and gives attachment to the tentorium cerebelli along this groove. The posterior border has a gutter for the inferior petrosal sinus. At the junction of the petrous and squamous parts are two canals separated by a thin bone; the upper canal contains the tensor tympani and the lower, the auditory canal (Fig. 7.2).
♦ Etiology
The causes of facial nerve palsy vary. Blunt head trauma in motor vehicle accidents or from gunshot wounds is responsible for the majority of lesions. Other causes include penetrating stab wounds and operative trauma. Symmetric middle cranial neuropathies can result from crushing injuries of the skull. Blunt head trauma is accompanied by basilar fractures and involves the cranial nerves near the fractures. In gunshot wounds the bullet has a trajectory—horizontal in suicidal attempts and anteroposterior in homicidal injuries. Avulsion and stretching of the nerve roots can occur with acceleration and deceleration trauma and in blunt injuries. These forces damage the nerves at their points of fixation or angulation.3,4 Minor trauma may precipitate palsy in a nerve previously stretched by tumors.5
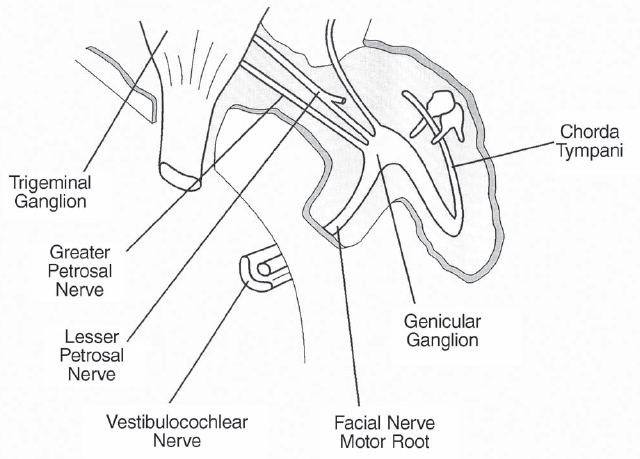
Fig. 7.1 Normal course of facial nerve within the temporal bone. The loop makes the nerve more susceptible whenever the temporal bone is fractured.
♦ Epidemiology
The incidence of cranial nerve injury varies by age group and demographics. Keane and Baloh6 provide a comparative tabulation of the incidence of cranial nerve injury after trauma. Facial and eighth nerve injuries have the greatest incidence, closely followed by temporal bone fractures.7,8 Road accidents are responsible for 50% of temporal bone fractures, and nearly 22% of all skull fractures are of the temporal bone; 7 to 8% of the latter have associated facial nerve injury.9,10 The association between types of temporal bone fracture and facial nerve injury is described in detail below.
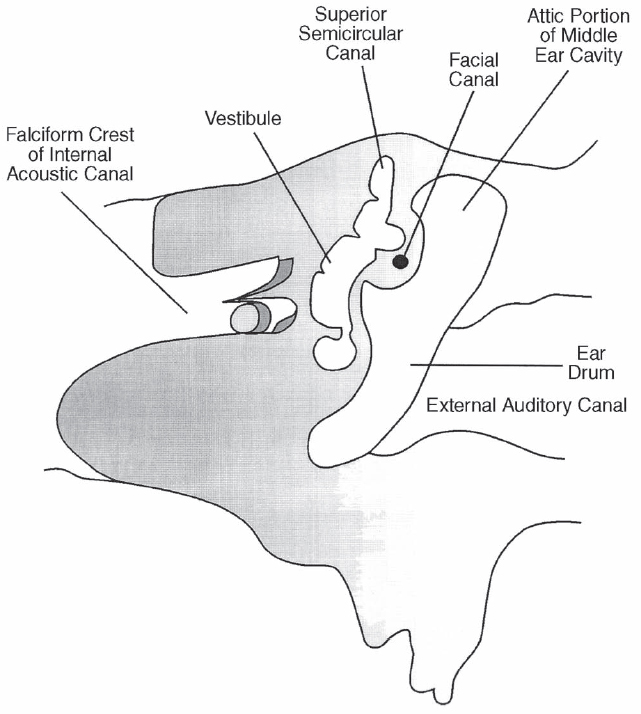
Fig. 7.2 A cross section of the petrous temporal bone with its contents. Because of the close anatomic proximity, temporal bone fracture result in injury to cranial nerves VII and VIII and the contents of the inner and middle ears.
♦ Clinical Manifestations
In general, the olfactory, facial, and vestibulocochlear nerves are damaged most frequently following blunt head trauma, with the lower cranial nerves (IX, X, XI, and XII) being the least commonly injured.11,12 In children younger than 10 years of age, the abducent and facial nerves are commonly injured.13 Because of the close proximity of the facial nerve with the vestibulocochlear nerve, the combination of hearing loss with facial nerve paralysis might be seen in cases of middle cranial fossa fractures with cerebrospinal fluid fistula. Although a facial nerve lesion is easily detected, manifestation of vestibulocochlear nerve injury in states of obtunded sensorium may be delayed. However, maintaining a strong clinical suspicion helps in detecting such combinations early. The type of temporal bone fracture sometimes correlates very well with the nerve lesions.14 The various degrees of facial nerve paralysis are described by House and Brackmann in their classification system. By and large, traumatic injury of facial nerve in the temporal bone produces infranuclear palsy (also known as Bell’s palsy).
♦ Etiopathologic Correlation Between Facial Nerve Injury and Temporal Bone Fractures
The long, tortuous, intraosseous course of the facial nerve in the temporal bone makes this nerve highly susceptible to injury in temporal bone fractures (Fig. 7.3). It is also injured in penetrating and blunt trauma to the head and face. Middle ear injury due to penetrating objects can easily damage this nerve. In approximately 50% of cases of transverse temporal bone fractures, the facial nerve within the internal auditory canal is damaged.9 With longitudinal fractures, the nerve is not directly involved, but a delayed paralysis may ensue secondary to edema, and facial nerve injury is seen in nearly 20% of cases. Temporal bone fractures are classified as transverse, longitudinal, and mixed, based on the relation of the fracture line to the axis of petrous pyramid.14
Longitudinal fractures follow a blow to the temporoparietal bone and start from a weak point in the squama or the mastoid part of the temporal bone. They constitute approximately 80% of all temporal bone fractures and present with the classic Battle’s sign of bloody otorrhea and a bony step-off in the external auditory canal. The fracture line traverses anteromedially through the middle ear, disrupts the ossicular chain, and is deflected anteriorly by the hard otic capsule. It may terminate in the middle cranial fossa or extend medially to the sphenoid bone, crossing the midline in 30% of cases.
Transverse fractures account for only 20% of temporal bone injuries. These require a force great enough to break the occipital bone at the foramen magnum, reaching the petrous pyramid. The intensity of such a force usually causes severe brain damage and disrupts the tough otic capsule, damaging both vestibular and cochlear components of the labyrinth. This fracture line generally spares the middle ear and has fewer external otologic findings. Facial nerve injury occurs in approximately 50% of cases, and the labyrinth is usually damaged by the fracture.
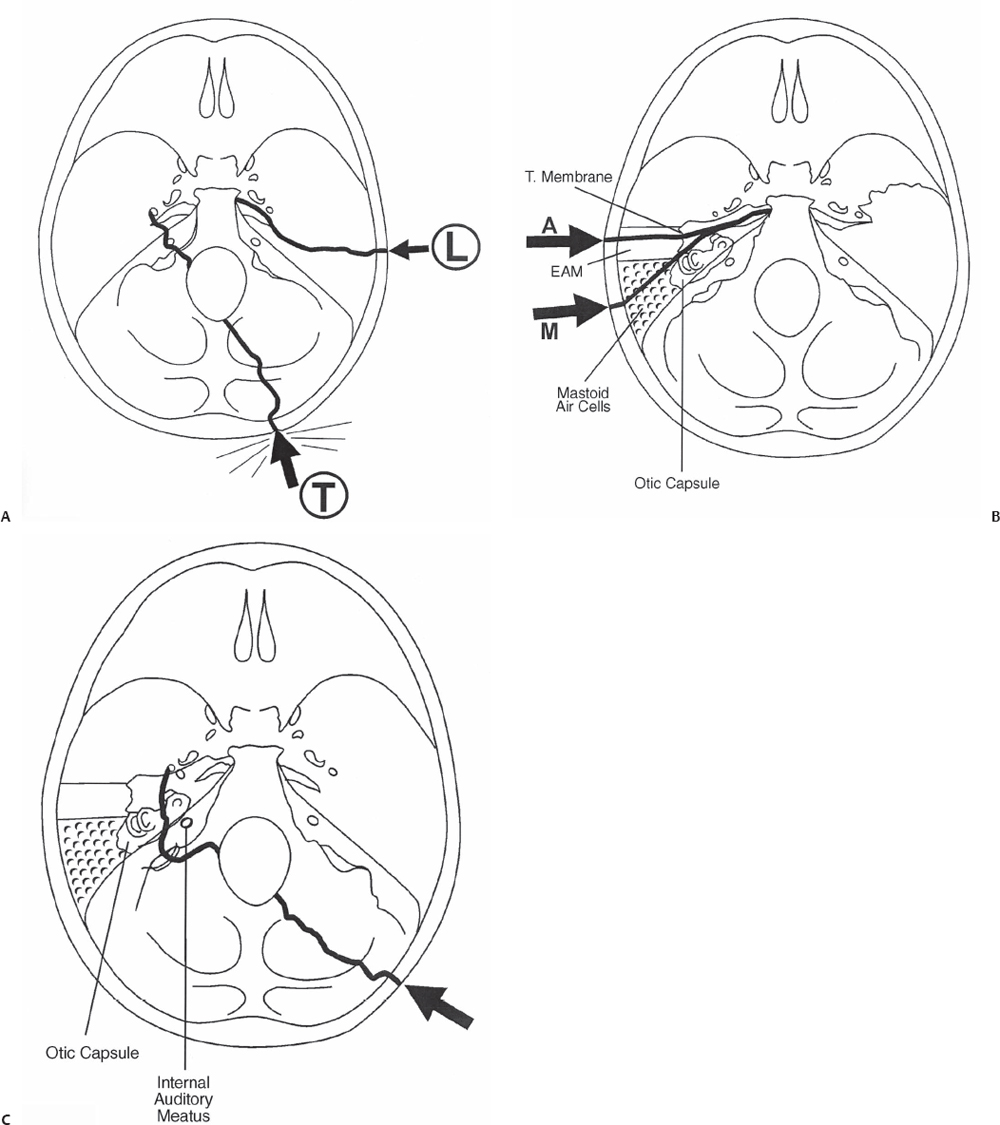
Fig. 7.3 (A) The types of temporal bone fractures. The arrow points to the area of impact to create the tangent of force for a given fracture. The weak squama of the temporal bone requires relatively a small force to yield and produce a longitudinal fracture (L), which runs parallel to the length of the petrous pyramid. This courses along the weak areas, such as air cells, the middle ear cavity, and skull base foramina. In contrast, a greater force is required along the thick occipital bone traversing the thick structure of the posterior cranial fossa to produce a transverse fracture (T) of the petrous bone rupturing the hard otic capsule also. (B) The longitudinal temporal bone fracture originates in the weak squamous temporal bone either the external auditory canal (A) anteriorly or the air cells of the mastoid sinus (M) posteriorly. With an anteriorly placed fracture, the tympanic membrane is ruptured, resulting in bloody otorrhea, whereas posterior fractures present with Battle’s sign and an intact tympanic membrane. The fractures course along the middle ear and reach the foramen lacerum deflected by the tough otic capsule, thus sparing the inner ear. (C) The transverse fracture requiring much greater force originates in the thick occiput bone and reaches the foramen magnum from where the force reaches the floor of the middle cranial fossa, fracturing the petrous pyramid perpendicular to its long axis, disrupting the otic capsule, thus damaging the inner ear and facial nerve. The fracture sometimes can pass lateral or medial to the otic capsule. With the medial course of the fracture, the internal auditory canal and its contents are at risk.
Mixed fractures have a combination of these findings and are thought to be less common. However, 65 to 80% of fractures have been reported to be neither longitudinal nor transverse, with the fracture lines traversing the petrous pyramid in an oblique way.15 Severe head injury can also avulse the nerve root from the brainstem; the patient usually has features of brainstem dysfunction. Facial paralysis is usually striking in cases of infranuclear paralysis. Injury to the vertical mastoid segment produces loss of taste on the ipsilateral anterior two thirds of the tongue. A horizontal segment (middle ear portion of the facial nerve) injury results in loss of the stapedius reflex (hypersensitivity to loud sound) and ipsilateral taste. Additionally, a lesion of the labyrinthine segment results in impaired ipsilateral lacrimation. Trauma involving the internal auditory canal injures both the facial and the vestibulocochlear nerves, and facial nerve symptoms, loss of hearing, and vertigo are present.14
♦ Grading of Facial Nerve Dysfunction
House and Brackmann proposed the clinical grading for facial nerve function (Table 7.1), originally intended for facial nerve paralysis and recovery in vestibular schwannoma treatment.
♦ Differential Diagnosis
Traumatic cranial neuropathy is a difficult diagnosis and requires continuous and repeat examination in cases with high-risk factors, including basal skull fracture, bleeding from the nose or ear, and orbital injury. As an exception, facial nerve paralysis may be easy to diagnose in comatose patients compared with other cranial nerve deficits. Facial paralysis in coma may be incidental and preexisting. A stroke-like presentation of head injury with upper motor neuron facial paralysis needs to be considered in cases where correlation is difficult. Neuroelectrophysiologic studies are helpful in these instances.
♦ Diagnostic Workup
Clinical suspicion is the best diagnostic tool in dealing with trauma. High-risk factors include basal skull fractures, which are best demonstrated by high-resolution computed tomography (CT) scan with thin slices. A good correlation exists between facial nerve injury or eighth nerve injury and type of temporal bone fracture.9 For both of these nerves, electrophysiologic monitoring is very useful in determining the diagnosis and prognosis of the injuries.6 Magnetic resonance imaging (MRI) is currently utilized to visualize the cranial nerves. Contrast-enhanced MRI can reveal facial nerve lesions including clinically silent traumatic lesions. Enhancement of the distal intrameatal and labyrinthine segments is described as specific for facial nerve palsy.17
Table 7.1 House and Brackmann Clinical Grading for Facial Nerve Function16
Grade 1: Normal: normal facial function in all areas | |
Grade 2: Mild dysfunction | |
| A. | Gross: slight weakness noticeable on close inspection, may have very slight synkinesis |
| B. | At rest: normal symmetry and tone |
| C. | Motion: |
| Forehead: slight to moderate movement | |
| Eye: complete closure with effort | |
| Mouth: slight asymmetry | |
Grade 3: Moderate dysfunction | |
| A. | Gross: obvious but not disfiguring asymmetry, noticeable but not severe synkinesis |
| B. | Motion: |
| Forehead: slight to moderate movement | |
| Eye: complete closure with effort | |
| Mouth: slightly weak with maximum effort | |
Grade 4: Moderate to severe dysfunction | |
| A. | Gross: obvious weakness and/or asymmetry |
| B. | Motion: |
| Forehead: none | |
| Eye: incomplete closure | |
| Mouth: asymmetry with maximum effort | |
Grade 5: Severe dysfunction | |
| A. | Gross: only barely perceptible motion |
| B. | At rest: asymmetry |
| C. | Motion: |
| Forehead: none | |
| Eye: incomplete closure | |
Grade 6: Complete paralysis: no movement | |
Grades 1 to 3 are associated with acceptable function | |
♦ Biologic Basis
The common forms of direct injury to the cranial nerves are stretch injury, contusion, laceration, and disruption. Trauma to the vicinity of a cranial nerve leads to delayed injury, resulting in compression of the nerve or edema of the nerve within its coverings. Indirect injury can also be vascular, with resultant ischemia that is either transient or permanent with thrombosis or disruption of blood vessels. Necrosis of the nerve cells follows acute and irreversible injury. In the early stages, the neurons shrink and the Nissl substance stains are relatively normal. Many necrotic neurons are than removed by phagocytes to form microglial nodules. Cavitation follows as the surrounding tissues become involved in the degeneration. Fragmentation and disappearance of the endoplasmic reticulum and disappearance of the Golgi apparatus follow dissolution of the Nissl bodies. Later, cytoplasmic membranes and ribosomes disappear and mitochondria are disrupted. These changes are accompanied by vascular congestion and perivascular inflammation. Phagocytes engulf these necrotic neurons, and soon the nerve fibers show changes of degeneration, usually within 3 days of the death of their corresponding cell bodies.
♦ Management
High-resolution CT is indicated in all cases of facial nerve trauma. In the initial stages of trauma with cerebrospinal fluid (CSF) otorrhea, judicious use of diuretics and proper positioning help reduce the leak. Usually prophylactic antibiotics are not indicated, unless surgical intervention is planned. Electrophysiologic monitoring is preferred, as an excellent spontaneous recovery can be expected with delayed-onset paralysis. With nonsurgical management, 90% of patients experience good recovery within 6 months.18 Absent facial nerve stimulation after 4 days may indicate the need for surgical exploration, especially with transverse fractures of the temporal bone and a discontinuous fallopian canal. Available electrodiagnostic tests that are used to evaluate facial nerve injury examine the nerve distal to the stylomastoid foramen. These tests cannot evaluate the nerve across the injury site because the nerve is mostly injured within the temporal bone. Harl and McPhee19 therefore suggested transcranial magnetic stimulation of the nerve, proximal to the injury site. They found that such stimulation was able to assess the integrity of the nerve after trauma and could predict the potential for functional recovery. These methods, however, are still at an experimental stage. The early return of voluntary motor potentials on standard electromyography carries a favorable prognosis.
Facial nerve decompression surgery should be considered for patients showing more than 90% denervation within 6 days after the onset of palsy.20 A mastoidectomy and decompression of the nerve under microsurgical techniques with or without repair using grafts may be beneficial.21,22 Decompression surgery usually has a beneficial effect when performed within 14 days of injury, and late surgery is recommended in bad head injury cases and in patients who do not exhibit recovery of facial nerve function.23 Beneficial effects of decompression may be seen even in patients who present 1 to 3 months after injury with more than 95% denervation on electroneuronography.
The surgical approach depends on the hearing status. With preserved hearing, a transmastoid (extralabyrinthine) approach is indicated when the tympanic and mastoid segments of the facial nerve need to be inspected, whereas a middle cranial fossa approach is appropriate for the geniculate ganglion and labyrinthine regions. A translabyrinthine approach provides access to the entire intratemporal facial nerve, in cases with hearing loss.24
Adjuvant therapy entails the application of natural tears and Lacri-Lube and is indicated if eye closure is impaired. In cases of complete facial nerve palsy with fifth nerve impairment, early tarsorrhaphy would be preferable to prevent corneal ulcerations and subsequent complications leading to phthisis bulbi.
♦ Anesthesia
Surgical treatment is required in selective acute situations, and anesthesia follows routine trauma protocol, except for an allowance for intraoperative neuroelectrophysiologic monitoring where ultra–short-acting muscle relaxants and inhalation anesthetics are favored.
♦ Prognosis
A positive percutaneous stimulation after 4 days of facial nerve trauma indicates excellent prognosis for recovery. In most cases, facial palsy makes a good spontaneous recovery. In patients with deteriorating facial nerve injuries as demonstrated by electroneuronography, surgical exploration is indicated. Primary end-to-end neurorrhaphy is the preferred management for transection injuries, whereas facial nerve decompression may benefit other forms of high-grade nerve trauma. Recovery of satisfactory nerve function can be expected in 75% of cases treated within 3 months after trauma.24
Facial reanimation is performed (e.g., hypoglossal-facial anastomosis) after 1 to 2 months, if the facial nerve is divided or after 1 year if no function returns before that time. In these cases with delayed presentations, secondary facial reanimation procedures, such as cranial nerve crossovers, dynamic muscle slings, or various static procedures, are useful adjuncts.25
References
1. Rucker CW. The causes of paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol 1966;61(5 Pt 2):1293–1298 PubMed
2. Elsberg CA. The Edwin Smith Surgical Papyrus and the diagnosis and treatment of injuries to the skull and spine 5000 years ago. Ann Med Hist 1931;3:271–279
3. Rovit RL, Murali R. Injuries of the cranial nerves. In: Cooper PR, ed. Head Injury, 3rd ed. Baltimore: Williams & Wilkins, 1993:183–202
4. Carter DA, Mehelas TJ, Savolaine ER, Dougherty LS. Basal skull fracture with traumatic polycranial neuropathy and occluded left carotid artery: significance of fractures along the course of the carotid artery. J Trauma 1998;44:230–235 PubMed
5. Eyster EF, Hoyt WF, Wilson CB. Oculomotor palsy from minor head trauma. An initial sign of basal intracranial tumor. JAMA 1972;220: 1083–1086 PubMed
6. Keane JR, Baloh RW. Posttraumatic cranial neuropathies. Neurol Clin 1992;10:849–867 PubMed
7. Russell WR. Injury to cranial nerves and optic chiasm. In: Brock S, ed. Injuries of the Brain and Spinal Cord and Their Coverings, 4th ed. New York: Springer-Verlag, 1960
8. Ghorayeb BY, Yeakley JW, Hall JW III, Jones BE. Unusual complications of temporal bone fractures. Arch Otolaryngol Head Neck Surg 1987;113: 749–753 PubMed
9. Cannon CR, Jahrsdoerfer RA. Temporal bone fractures. Review of 90 cases. Arch Otolaryngol 1983;109:285–288 PubMed
10. Brodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. Am J Otol 1997;18:188–197 PubMed
11. Turner J. Indirect injuries of the optic nerve. Brain 1943;66:140–151
12. Gurdjian ES, Webster JE. Head Injuries: Mechanisms, Diagnosis and Management. Boston: Little, Brown, 1958
13. Kitchens JL, Groff DB, Nagaraj HS, Fallat ME. Basilar skull fractures in childhood with cranial nerve involvement. J Pediatr Surg 1991;26:992–994 PubMed
14. Blevins N, Jackler R. Facial, auditory and vestibular nerve injuries associated with basilar skull fractures. In: Youmans J, ed. Neurological Surgery, Vol 3. Philadelphia: WB Saunders, 1996:1865–1878
15. Ghorayeb BY, Yeakley JW. Temporal bone fractures: longitudinal or oblique? The case for oblique temporal bone fractures. Laryngoscope 1992;102:129–134 PubMed
16. House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg 1985;93:146–147 PubMed
17. Kinoshita T, Ishii K, Okitsu T, Okudera T, Ogawa T. Facial nerve palsy: evaluation by contrast-enhanced MR imaging. Clin Radiol 2001;56:926–932 PubMed
18. May M. Trauma to the facial nerve. Otolaryngol Clin North Am 1983; 16:661–670 PubMed
19. Har-El G, McPhee JR. Transcranial magnetic stimulation in acute facial nerve injury. Laryngoscope 2000;110:1105–1111 PubMed
20. Fisch U. Prognostic value of electrical tests in acute facial paralysis. Am J Otol 1984;5:494–498 PubMed
21. Glasscock ME III, Wiet RJ, Jackson CG, Dickins JR. Rehabilitation of the face following traumatic injury to the facial nerve. Laryngoscope 1979; 89(9 Pt 1):1389–1404 PubMed
22. Lambert PR, Brackmann DE. Facial paralysis in longitudinal temporal bone fractures: a review of 26 cases. Laryngoscope 1984;94:1022–1026 PubMed
23. Chang CYI, Cass SP. Management of facial nerve injury due to temporal bone trauma. Am J Otol 1999;20:96–114 PubMed
24. Quaranta A, Campobasso G, Piazza F, Quaranta N, Salonna I. Facial nerve paralysis in temporal bone fractures: outcomes after late decompression surgery. Acta Otolaryngol 2001;121:652–655 PubMed
25. Davis RE, Telischi FF. Traumatic facial nerve injuries: review of diagnosis and treatment. J Craniomaxillofac Trauma 1995;1:30–41 PubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








