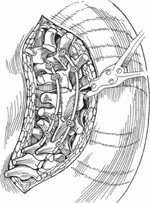
60 Timothy R. Kuklo and Alexander R. Vaccaro Severe rigid spinal deformity is a difficult problem for the spinal surgeon (Fig. 60.1). The traditional approach to severe rigid spinal deformities has included a stabilizing posterior spinal fusion with instrumentation, or an anterior release and fusion followed by a posterior spinal fusion with segmental instrumentation. Both of these approaches have resulted in variable, but mostly limited, correction, as a true translation of the spinal column is limited by these approaches. Vertebral column resection (VCR) is the only means of achieving significant vertebral column translation in these difficult deformities. It has traditionally been most commonly utilized for congenital scoliosis. Fig. 60.1 A posterior view of a severe coronal plane deformity. Vertebral column resection implies complete resection of the posterior elements, pedicles, and the entire vertebral body. It can be achieved through either an anterior-posterior approach (on a single day or staged), or through a posterior only approach. Generally, VCR does not result in direct bone-on-bone contact, as is common with Smith-Petersen and pedicle subtraction osteotomies; therefore, reconstruction of the anterior and posterior columns is required. As well, the procedure is considered a vertebral column shortening procedure. Compromised pulmonary function, which is frequently encountered, may be a contraindication to an anterior approach, and thus may tip the surgeon toward a posterior-only VCR. The posterior-only procedure, however, is more technically demanding. Mastery of an anterior-posterior VCR is necessary prior to attempting a posterior-only VCR. The larger the resection, the greater the associated blood loss, risk of neurologic deficit, and other significant complications. Vertebral column resection is indicated for any severe fixed deformity, such as: The most dominant aspect of the clinical presentation is often sagittal plane decompensation; however, patients generally complain of difficulty with standing or sitting secondary to pelvic obliquity with imbalance, apparent leg-length discrepancy, and cosmetic concerns. After evaluation of the deformity, consideration should be given to the surgical approach, technique (i.e., multiple Smith-Petersen osteotomies, pedicle subtraction osteotomy, or vertebral column resection), levels of resection, and levels of instrumentation. A VCR is not recommended for medically compromised patients who cannot undergo an extended period of anesthesia or potentially significant blood loss, as the procedure can entail extended operative time or excessive blood loss. Like other procedures, spinal instrumentation is generally contraindicated with active infection. A thorough understanding of the complexity of the multiplanar deformity is mandatory. Ideally, this should be evaluated with a complete radiographic scoliosis series (standing anteroposterior [AP], lateral, side-bending, and hyperextension lateral over a bolster) if possible. This series assists the surgeon in assessing the potential flexibility of the deformity, as well as overall sagittal and coronal decompensation. If standing radiographs are unobtainable, then sitting AP and lateral radiographs should be obtained. Further radiographic evaluation should also include a thin-section computed tomography (CT) scan with sagittal, coronal, and three-dimensional (3D) reconstructions. The CT images greatly assist in defining and understanding the bony anatomy and in assisting with preoperative planning. The CT also assesses pedicle size and location, and postoperative screw placement. Magnetic resonance imaging (MRI) is helpful in assessing associated spinal canal abnormalities, especially in congenital scoliosis, as well as in detecting potential areas of central or foraminal stenosis. For an anterior-posterior vertebral column resection, the patient is placed in the lateral decubitus position on a bean bag with an axillary roll, usually the right lateral decubitus (left-side approach) on a radiolucent table. Following this, the patient is flipped to the prone position on an open Jackson frame. For a posterior-only VCR, the patient is placed directly in the prone position on a well-padded radiolucent table. The arms are placed with the shoulders abducted 90 degrees and the elbows are flexed 90 degrees. General anesthesia is used, and the neck is placed in a neutral to slightly flexed position. Generally, only one or two vertebrae are necessarily resected along with the associated disks (three disks for two-level resection), especially for sharply angulated deformities. This is determined by both the magnitude of the deformity, as well as the acuteness of the angulation. For long sweeping rigid curves, more than one vertebra may need to be resected. In either case, the goal is to achieve a balanced correction without stretching or compressing the spinal cord. With potentially large expected blood loss, all efforts should be made to control bleeding from the onset of the procedure. This includes meticulous dissection and control of soft tissue bleeders, with liberal use of powdered thrombin-soaked Gelfoam (Pharmicia & Upjohn Company, Kalamazoo, MI), or similar available commercial products such as FloSeal (Baxter Healthcare Corporation, Fremont, CA). For tumor resections, consideration should be given to preoperative arterial embolization; however, this may also increase the risk of spinal cord compromise or loss of function secondary to the embolization. As well, it is recommended to keep the blood pressure at the resting mean arterial pressure during correction, and to closely watch for an acute drop in pressure during correction. Spinal cord monitoring, specifically somatosensory and motor evoked potentials, should also be closely watched during correction. After correction, a wake-up test should be considered. Inherent to this is a close working relationship with the anesthesia team. The most important difficulty encountered is compromised neurologic function during or following VCR. Consequently, meticulous attention to complete visualization, and slow steady correction, as outlined above, are mandatory. As well, VCR is an inherently destabilizing procedure; therefore, rigid internal fixation with at least two or three levels of fixation is required both proximal and distal to the level of resection. Attention should also be given to the condition of the bone, as osteoporotic or compromised bone quality may necessitate additional levels of fixation. As well, pseudarthrosis or loss of fixation are significant concerns. Persistent imbalance or loss of lumbar lordosis may also be encountered during the correctional procedure. Small pedicles, which make pedicle screw fixation difficult, may be particularly difficult to identify, and alternative fixation strategies should be considered at these levels if it is thought to be a critical level of fixation. The anterior procedure is done through either a thoracotomy or thoracoabdominal approach on the convex side of the deformity. An anterior osteotomy is performed if there is a solid fusion. Ideally, an osteoperiosteal flap is elevated, but this is often too difficult. Often the area to be resected is removed to the level of the adjacent disk, which is also removed along with the articular cartilage of the adjacent end plate back to a bleeding subchondral bone. All of the bone back to the posterior longitudinal ligament (PLL) is removed piecemeal. It is optional to remove the PLL, as infolding of the PLL into the spinal canal could result in spinal cord compression during a correctional maneuver. The entire vertebral body, and convex pedicle are removed. A lamina spreader is helpful to maintain or improve visualization of the area to be resected; however, overdistraction should not be applied. After complete resection, an autologous tricortical iliac crest, femoral allograft, titanium mesh with allograft or autograft, or an expandable cage is placed. Whatever the chosen interbody spacer, a vertebral column shortening will be the ultimate final corrected spinal alignment. Instrumentation is often applied following grafting. The patient is then flipped to the prone position for a posterior element resection and segmental instrumentation, or returned at a later date for this procedure (Fig. 60.2).
Vertebral Column Resection
Description

Key Principles
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Anterior-Posterior (Circumferential) Vertebral Column Resection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







