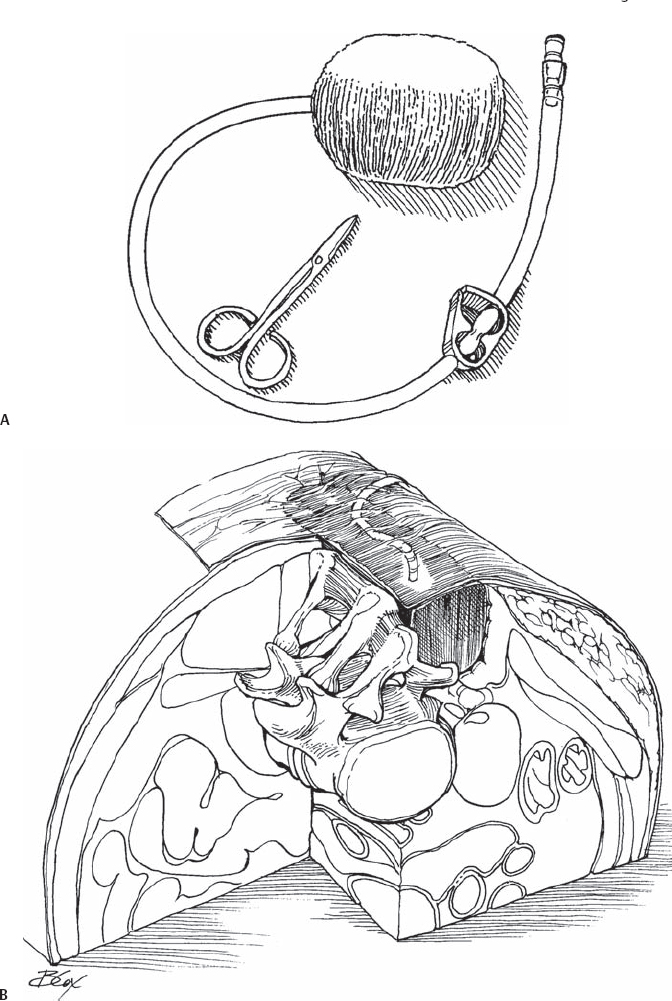
81 John M. Beiner and Linda Mascolo Traditional management of postoperative spinal (or bone graft donor site) wound infections, consisting of repeated operative debridement or bedside dressing changes, has largely been supplanted by the use of closed-system suction devices known as wound Vacuum Assisted Closures (VACs). This system consists of a specifically designed sponge that is placed into the infected wound bed, covered by an adhesive, occlusive drape, with suction applied via a vacuum device to promote wound healing, decrease wound size, help remove interstitial fluid allowing tissue decompression, improve perfusion, and assist in the removal of infectious materials (Fig. 81.1). Fig. 81.1 (A) Typical components of the wound vacuum assisted closure packs: black sponge, tubing, and scissors. (B) Close-up of a wound with the component layers in place (from inside out): sponge, suction tubing, and occlusive layer. Generalized wound treatment principles should be emphasized. Necrotic tissue and purulent fluid must be removed, and an abscess cannot be treated with anything other than operative debridement. Once the gross bacterial load has been reduced, the wound can begin to form granulation tissue. Adequate nutrition (prealbumin above 15 mg/dL) must be stressed. The wound VAC (KCI, San Antonio, TX) can speed closure of an infected spinal or bone graft site wound. The wound VAC is expected to shorten time to healing, encourage granulation tissue formation, and reduce the need for repeat trips to the operating room with their attendant risks, (anesthesia, nutritional depletion, and blood loss) as well as decrease hospital length of stay. Once all gross purulence and necrotic tissue have been removed, the VAC should be applied and changed every 48 hours. The expected outcomes of this therapy are to promote an environment for healthy granulation tissue growth, decrease bacterial colonization, and improve time to wound closure or graft. Postoperative posterior spinal wound infections, iliac crest wound infections, or de novo spinal infections, once adequate debridement has been performed. The wound VAC also has clinical applications throughout the surgical arena for soft tissue loss and infections. Active CSF leak. The wound VAC in this setting can contribute to the formation of a pseudomeningocele. Some animal studies have shown that exposed bone should be decorticated to encourage granulation tissue to form. If exposed dura is present, suction may be decreased to 75 to 100 mm Hg; any radicular sensation may indicate excessive suction causing neural irritation. VAC vers-foam, a dense hydrophilic foam (white in color) is a nonadherent material that helps protect delicate structures and should be placed deep to the fascia on top of the dura. Granufoam, a reticulated hydrophobic foam (the black sponge) may then be placed superficial to this to allow a relative gradient in suction to protect the dura. Wounds below the fascial level may necessitate conscious sedation for removal and changing of the sponge. This decreases apprehension in patients who may already be frustrated with their infection, and allows a better debridement of tissue. This may be arranged in the operating room, the recovery room, or an intensive care unit. Alternatively, saline may be used to moisten the sponge to allow it to be removed more easily. Lidocaine can also be injected into the sponge prior to removal, as a topical anesthetic to improve pain control during the dressing change. With wounds superficial to the fascia, bedside changes are often well tolerated. The VAC should be placed only into a relatively clean wound; it will not draw interstitial fluid and bacteria away from necrosis or purulence. It is important that the foam dressing be placed in the wound covering the entire wound base and sides, tunnels, and undermining; packing only superficially will encourage the fascia to close prematurely and may cause the treatment to fail. If purulent material is noted with the packing change, the surgeon should resort to repeated operative debridement or saline gauze wet to dry dressing changes until the wound is clean prior to reapplication of the VAC. Staff members may be reluctant to fully pack the sponge into the cavity. The sponge should be cut to the contour of the soft tissue deficit, but not packed into compression. Because this often generates significant pain in subfascial wounds, the resident, nurse, or physician’s assistant is often reluctant to pack deep enough. A responsible care provider should personally supervise most VAC dressing changes, preferably with the skin/wound care nurse who is available at many hospitals, to ensure that healing is progressing from inside out, with no pockets forming. Operative debridement should occur until the wound is clean. The sponge is then contoured and placed into the soft tissue defect (often at the time of the last operative debridement), followed by an occlusive adherent dressing. A hole is then cut into the middle of this dressing, allowing placement of the suction/ therapeutic regulated accurate care (TRAC) (KCI, San Antonio, TX) pad over this hole. The tubing may then be supported with more sponge and adhesive dressing to secure it to the skin in a convenient position to prevent pain from “laying on the tubing” and to allow improved patient mobilization. The wound edges may be “window-paned” with a hydrocolloid dressing (Duoderm) to protect the skin from shear stress. Suction is then applied: 125 mm Hg for most cases, but see above for exceptions. The dressing should be changed and assessed every 48 hours. Saline wet to dry dressing changes, “feed me-drain me” irrigation systems, or silver-impregnated VAC sponges can be used for resistant infections. Hardware removal is rarely necessary.
Wound Vacuum Assisted Closures (VAC) Management for Spinal or Bone Graft Wound Infections
Description
Key Principles
Expectations
Indications
Contraindications
Relative Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Bailout, Rescue, Salvage Procedures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








