48
Anterior Lumbar Interbody Fusion (ALIF): Cylinder Cages, Femoral Ring Allograft, Trapezoidal Synthetic Implants
Arya Nick Shamie
Description
Using the anterior retroperitoneal, transperitoneal, or lateral trans-psoas approach, the disk space is exposed. A complete diskectomy is performed and an implant is used to distract the end plates, create annular tension, and accomplish a fusion of the disk space. Autogenous bone graft, bone marrow, biologics, or bone morphogenetic protein (BMP) is used to increase the fusion rate.
Expectations
Anterior lumbar interbody fusion (ALIF) exposure allows for a near-complete diskectomy. This anterior exposure allows for a larger implant with a greater area of contact with the end plates as compared with smaller, posteriorly placed interbody implants. Therefore, less risk of subsidence and higher fusion rates are expected. BMP implantation not only increases the fusion rates as comparable to autogenous bone graft but also avoids the morbidity associated with the bone graft harvest site. ALIF avoids the exposure through the posterior musculature and the “fusion disease” associated with it.
Indications
Discogenic back pain with positive diskogram, instability, or grade one spondylolisthesis, pseudarthrosis, or continued back pain following a posterolateral fusion. Relative indication includes revision of failed spine arthroplasty.
Contraindications
Multilevel discogenic back pain, spinal canal pathology, osteoporotic bone, bone-on-bone degenerative disk disease, instability with greater than 25% listhesis in any direction. Relative contraindications include prior retroperitoneal surgery with adhesions, and a young male patient.
Special Considerations
Anterior lumbar interbody fusion in osteoporotic patients should be avoided. Complete diskectomy and exposure of the underlying bleeding end plates improve fusion rates. Fixation with an anterior plate or pedicle screw fixation can also improve fusion rates. The use of BMP in cages is indicated for improved fusion rates.
Preoperative planning with templating of the operative level and the adjacent disk space is helpful to restore the appropriate disk height. Bifurcation of the great vessels can be visualized on magnetic resonance imaging (MRI), and hence the surgical approach can be individualized. Calcified great vessels visualized on preoperative radiographs should be retracted carefully to minimize the risk of a thrombotic event, which could compromise lower extremity perfusion.
The extreme lateral trans-psoas approach (XLIF) has its own unique considerations. Electromyograph (EMG) monitoring of the tubular dilators, as they are advanced through the psoas down to the disk space, is a requirement to avoid nerve root injury. XLIF is not generally possible at the L5-S1 level due to obstruction by the iliac wing. In rare cases, the XLIF procedure may need to be converted to an ALIF procedure due to anatomic limitations; patients should sign consent forms for both procedures when an XLIF is planned.
Tips, Pearls, and Lessons Learned
Lateral fluoroscopy versus spot radiography is helpful in identifying the disk space margins as the implant is seated in its ideal position. This ideal position is a few millimeters recessed deep to the anterior margin of the adjacent end plates. The osteophytes should be rongeured off the anterior end plates prior to the diskectomy as they may obscure normal anatomy and result in improper placement of the inter-body implant. Once the anterior annulus is incised with a scalpel, a Cobb elevator can be used to detach the Sharpey’s fibers from the superior and inferior end plates, and then the disk can be removed in one piece. Overly sclerotic end plates can be burred in the center to expose the bleeding end plates. Sequential dilation of the disk space with sizers is an important step to adequately distract the end plates and insert a press-fit implant. An AO cancellous screw with a washer can be placed at the anterior corner of the inferior end plate to minimize the risk of anteropulsion of the implant.
Key Procedural Steps
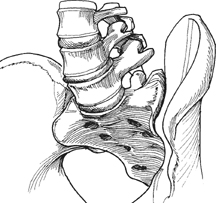
Direct Anterior Approach (Figs. 48.1 and 48.2)
This approach is typically used for the L5-S1 level, which is below the bifurcation of the great vessels. A Pfannenstiel incision is made, and the retroperitoneal approach to the disk space is accomplished. The middle sacral artery, which typically crosses the field, is dissected and ligated. The diskectomy and end-plate curetting to bleeding bone is performed and distractors followed by sizers are used for proper implant size selection. The implant is then packed with bone graft or BMP and is impacted into the disk space using fluoroscopy guidance. The implant can also be inserted while the patient’s lumbar spine is in hyperlordosis, created by patient positioning. The patient needs to be returned to neutral alignment after the implant is positioned to check for stability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







