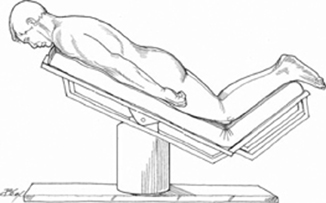
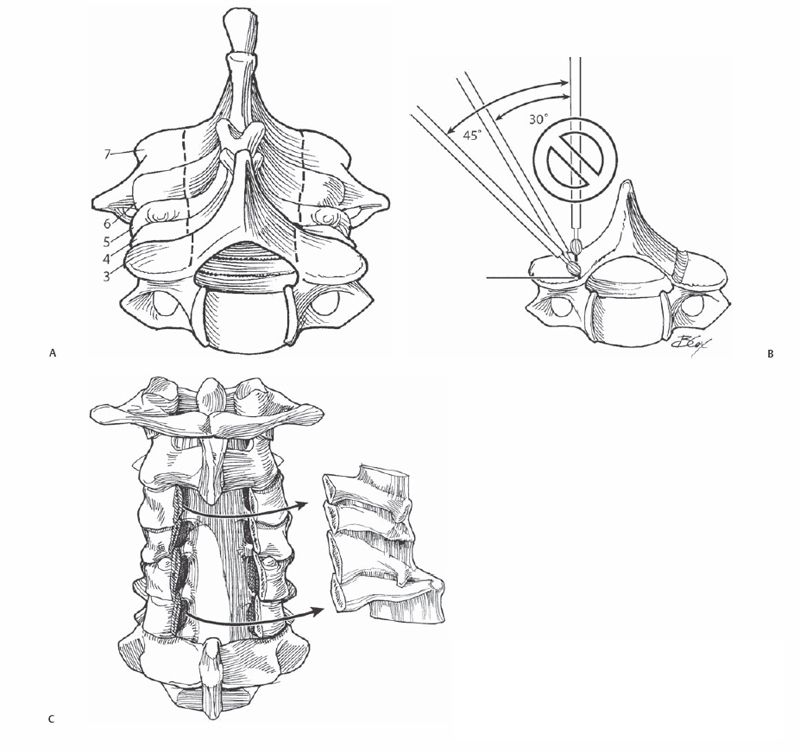
2 Brian Kwon and David H. Kim The removal of compressive bone and soft tissue structures surrounding the cervical spinal cord (laminectomy) or its nerve roots (foraminotomy). Laminectomy is used for expansion of the cervical canal in individuals with symptomatic cervical stenosis. This is typically found in individuals with spondylotic degeneration overlying developmentally narrow canals. Multilevel decompression can be easily accomplished through a simple posterior surgical approach. Foraminotomy can be performed as an independent procedure or in conjunction with laminectomy to address unilateral or bilateral single-level or multilevel foraminal stenosis caused by spondylotic osteophyte formation or soft disk herniations. Laminectomy performed for cervical myelopathy typically involves multilevel decompression. Recently laminectomy performed as a stand-alone procedure has fallen out of favor due to the incidence of postoperative kyphosis and recurrent symptoms. In current practice, laminectomy is more commonly performed with concomitant instrumented fusion. Clinical results in patients who are ambulatory preoperatively are generally favorable with most patients experiencing at least partial neurologic recovery. Foraminotomy yields good to excellent relief of arm pain in the majority of patients. Best results have been observed in single-level disease associated with lateral soft disk herniation. Kyphotic sagittal alignment. Medial pathology, i.e., disk herniation or compressive osteophyte, where surgical access may be associated with increased risk of neurological injury. Laminectomy requires lordotic or neutral alignment, measured from the superior end plate of C3 to the inferior end plate of C7 on upright cervical spine films. The number of levels included should be determined by the anatomic distribution of compressive pathology noted on magnetic resonance imaging (MRI) or computed tomography (CT) after myelography. Facet resection in excess of 50% during foraminotomy can lead to segmental instability. Preoperative lateral flexion/extension films are recommended to assess for the presence of instability. Fig. 2.1 Patient position on operating bed. Bed position should be in 30-degree reverse Trendelenburg, with the foot of the bed flexed 30 degrees to prevent migration of the patient toward the foot of the bed. For both procedures, patients can be positioned prone or seated. The seated position can facilitate surgery by decreasing blood loss, but may risk air embolism. Familiarity with this position is crucial for both surgical and anesthesia staff. The prone position on chest rolls is more widely utilized. The patient’s head can be secured with Mayfield tongs. While the patient is in the prone position, the eyes and nose should be protected and periodically checked. If possible, the head and neck should be placed in the “military position” without flexion or extension and slight posterior translation of the head. The use of neurophysiologic spinal cord monitoring is recommended in the setting of myelopathy. Baseline evoked potential signals should be obtained prior to patient positioning and then rechecked shortly after the patient has been placed in the final operative position. Arms are tucked at the sides. Gentle caudal traction can be placed on the shoulders with tape to help with radiographic visualization of the lower cervical levels, especially in individuals with broad or thick shoulders. Bed position should be in 30-degree reverse Trendelenburg, with the foot of the bed flexed 30 degrees to prevent migration of the patient toward the foot of the bed (Fig. 2.1). Hypotension should be avoided in myelopathic patients. In patients with myeloradiculopathy and significant radicular symptoms, the presence of significant foraminal stenosis should be sought on preoperative imaging studies and appropriate concomitant foraminotomies planned. In preoperative positioning, excessive flexion or extension should be avoided in myelopathic patients. For foraminotomies, slight kyphosis opens the interspaces and foramina, but care must be taken during dissection as the dural sac is more susceptible to injury. The surgical exposure for laminectomy proceeds caudal to rostral; this facilitates subperiosteal detachment of paraspinal muscles, which attach in the same direction and reduce bleeding. A clamp is placed on an exposed spinous process and a lateral radiograph is obtained to confirm levels. Dissection should proceed to the lateral margin of the facet joints. This extent of exposure establishes landmarks needed for safe placement of lateral mass screws and ensures that more than half of the facet joint is not removed during any associated foraminotomy. Dissection beyond the lateral margin risks significant bleeding from the soft tissue in this area. Care must be taken not to injure the facet capsules at any level where fusion is not planned. The epidural venous plexus surrounding the cervical cord can be severely compressed in myelopathic patients. Brisk bleeding can occur from the epidural plexus as well as the venous plexus surrounding the cervical nerve root within the neuroforamen following decompression. Careful bipolar coagulation or use of Surgicel can provide adequate hemostasis. Blind compression or coagulation can lead to serious nerve root or spinal cord injury and should be avoided. With the neck in neutral position, the ligamentum nuchae is relatively lax and tends to meander from the midline. Maintaining dorsal traction using hooks or retractors can facilitate midline dissection and reduce bleeding. Avoid detaching the muscular insertions from the cephalad border of the C2 spinous process. The cephalad and caudad border of each lamina should be carefully freed of soft tissue. Preparation of screw holes for implant placement should be performed prior to the actual laminectomy to minimize the risk of spinal cord injury. Laminectomy margins should be created 2 mm medial to the junction of the lamina and lateral mass using a 2-mm high-speed burr. This reduces bleeding from epidural vessels localized directly anterior to the junction of the laminae and lateral masses. In the setting of severe stenosis, sublaminar placement of instruments risks injury to the spinal cord and should be avoided. The angle of approach with the burr should be 30 to 45 degrees in the horizontal plane to avoid burring into the lateral mass (Fig. 2.2A,B). A gentle sweeping motion with the burr should be performed to gradually and evenly deepen the laminectomy trough. Once all laminae have been divided they can be removed en bloc by detaching the interspinous ligament and ligamentum flavum with a Kerrison rongeur or knife (Fig. 2.2C). Gentle dorsal traction is maintained on the detached laminae using towel clips on the individual spinous processes. To reduce the risk of postoperative C5 and C6 root palsy, a concomitant C5 and C6 foraminotomy is routinely performed. Once laminectomy has been completed, prior to rod placement, additional restoration of anatomic lordosis can be accomplished by loosening the Mayfield attachment and gently extending the patient’s neck.
Cervical Laminectomy and Foraminotomy
Description
Key Principles
Expectations
Indications
Laminectomy
Foraminotomy
Contraindications
Laminectomy
Foraminotomy
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








