24
Costotransversectomy
John E. Tis and Timothy R. Kuklo
Description
Several diseases of the spine require resection of all or part of the vertebral body and concurrent exposure of the posterior elements. These include some benign and malignant tumors that require biopsy or resection, congenital kyphosis and kyphoscoliosis, hemivertebra resection, and rigid scoliosis. The traditional approach has been to perform a combined anterior and posterior approach in a staged fashion. The anterior approach is necessary to remove all or part of the vertebral body, and the posterior approach is then performed to complete the resection of the posterior elements or provide stabilization with rigid posterior instrumentation. Costotransversectomy was first described by Menard to treat a paraspinal abscess associated with tuberculosis. Since then, it has also been described as a method to treat thoracic disk herniations, spinal nerve root tumors, ventrally based space-occupying intraspinal lesions, and all of the conditions listed above that have traditionally required anterior and posterior access to the spine. This approach provides adequate exposure of the anterior column to allow resection of the vertebral body and limited anterior fusion with visualization of the thecal sac to allow resection of anterior spinal tumors or prevent cord impingement during deformity correction.
Key Principles
Although costotransversectomy has been shown to have similar complication rates to anterior and combined anterior/posterior approaches in experienced hands, it is a technically challenging procedure associated with potentially significant blood loss. Surgeons should be experienced in both anterior and posterior approaches before attempting a costotransversectomy.
Indications
Vertebral column resection is indicated for any disease that requires exposure or removal of part or all of the anterior or middle columns of the thoracic spine, such as the following:
- Congenital kyphosis and kyphoscoliosis
- Rigid, large curve scoliosis requiring vertebral osteotomy
- Thoracic disk herniations
- Metastatic or primary tumors of the spine that require debulking or excision
- Anterior intraspinal tumors
- Paraspinal abscess drainage
It is especially indicated for anterior exposure in patients who cannot tolerate a thoracotomy such as the elderly, or other patients with limited pulmonary reserve and in those patients in whom the surgeon wishes to avoid contamination of the thoracic cavity.
Contraindications
Conditions that require extensive anterior exposure and fusion may be better approached through an anterior (transthoracic) approach.
Special Considerations
A thorough understanding of the three-dimensional anatomy of the thoracic spine and costovertebral articulation is essential. Each rib has bilateral superior and inferior costovertebral articulations that contribute to the thoracic spine’s inherent stability.
Preoperative planning includes obtaining adequate radiographs to localize the pathologic process to be approached and obtain a rib count so that the correct rib(s) will be removed at the time of surgery. In the case of certain tumor resections (renal cell carcinoma, hemangioma, hemangiosarcoma), consideration may be given to preoperative arterial embolization to reduce blood loss.
Special Instructions, Position, and Anesthesia
This approach has been described with the patient in either the prone or lateral decubitus position. We prefer the prone position, especially if concurrent posterior instrumentation is to be performed. The patient is placed on a well-padded open Jackson frame or radiolucent table in the prone position with the abdomen allowed to hang freely. The radiolucent table has the advantage of allowing rotation around the central longitudinal axis (“airplaning” the table). The arms are placed with the shoulders abducted 90 degrees and the elbows flexed 90 degrees. General endotracheal anesthesia is used, and the neck is placed in a neutral to slightly flexed position. Alternatively, a Wilson frame may be used on a radiolucent table. The frame is elevated to its maximum height during the exposure and resection, and lowered during instrumentation and deformity correction. Spinal cord monitoring is placed (somatosensory and motor evoked potentials), and central intravenous access is established along with an arterial line. Mean arterial pressure is kept at 70 mm Hg during the dissection and at the resting level during any deformity correction. The back is sterilely prepared and draped widely out to the posterior axillary line.
Tips, Pearls, and Lessons Learned
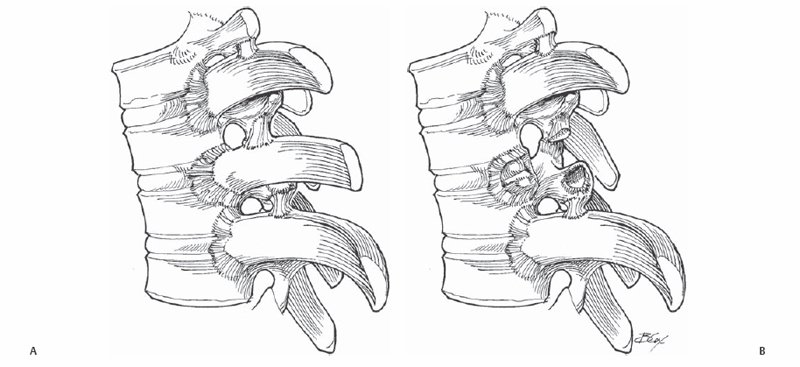
Removal of a rib head exposes the vertebra of the same number as well as the inferior portion of the adjacent, cephalad vertebral body (Fig. 24.1). Removal of the sixth rib head exposes the T5-T6 disk. Generally, only 2 to 4 cm of one or two ribs needs to be resected to allow access to the lateral aspect of two vertebrae. The rib heads to be resected should be at the level of the hemivertebra, disk, or tumor to be removed or the apex of the deformity. More extensive vertebral resections or more anterior dissection, such as that required for en bloc tumor resection, may require three or more ribs to be removed. The goal is to obtain adequate subperiosteal exposure of the vertebra(e) to be resected without violating the thoracic cavity. If more than three ribs are removed or bilateral resections are performed, this will cause instability requiring posterior instrumentation. If only a thoracic diskectomy is planned, the costovertebral joint and lateral end plates are drilled instead of performing rib resection. This allows limited exposure of the annulus that is sufficient to remove a single thoracic disk.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







