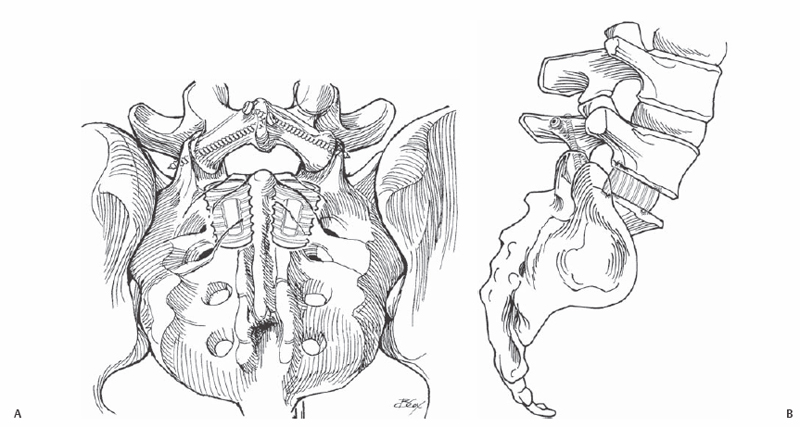
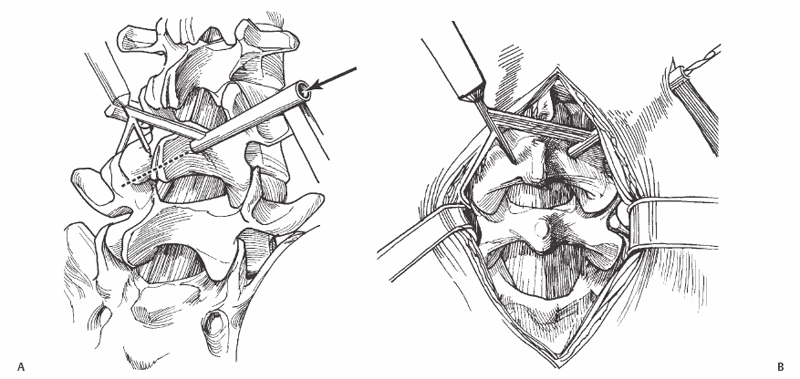
39 Eeric Truumees To safely stabilize a lumbar motion segment by placing screws across the facet joint. Translaminar facet screw (TLFS) fixation passes cortical screws, 50 to 60 mm in length by 4.5 mm in diameter, through the lamina into the facet via a 4-cm percutaneous approach. TLFSs are the lowest profile and least expensive of all posterior lumbar implants. Thus, the additional cost, bulk, muscular irritation and stripping, superior segment facet injury, and neurologic risk engendered by transpedicular instrumentation are avoided. Both anterior lumbar interbody (ALIF) and posterolateral lumbar (PLF) fusions are commonly utilized in the operative management of a wide variety of lumbosacral conditions. Given the high loads and limits of external immobilization, pseudarthrosis and clinical failure are common without instrumentation. As with other forms of lumbosacral fixation, TLFSs provide stability, thereby increasing the chance of successful fusion. These screws render the treated motion segment at least 2.4 times as stiff as an uninstrumented segment. In particular, TLFSs provide equal rotational and extension stability to transpedicular constructs. On the other hand, TLFSs are less strong in flexion. In that their mechanical strengths and weaknesses are exactly the opposite, they are ideally paired with cage reconstruction of the anterior column. Translaminar facet screws may be employed alone or as an adjunct to other forms of anterior or posterior instrumentation. Used alone, TLFSs are most commonly indicated for adjunctive fusion in stenosis patients with spondylolisthesis undergoing limited fenestration/laminotomy procedures. In some cases, the pedicles themselves are too small. Their use has been described in the stabilization of patients with pure ligamentous instability and in the management of pseudarthrosis in “stand-alone” ALIF patients. Translaminar facet screws may also be used as an adjunct to a transpedicular construct. For example, in multilevel reconstructions to the sacrum, screws into the wide sacral “pedicle” may provide inadequate fixation and construct failure may result. TLFSs may be used, with or without other adjunctive measures (e.g., anterior column support or alar screws), to improve segmental fixation at the lumbosacral junction. Most typically, TLFSs are used as an adjunct to cage fixation in patients undergoing ALIF (Fig. 39.1). While ring allografts and threaded, vertical mesh or horizontal interbody cages are ideal in resisting compressive, axial forces, they are inadequate in the neutralization of side bending, rotational, and extension forces. TLFSs function extremely well as an adjunct to these forms of anterior reconstruction by “locking in” the posterior elements. Fig. 39.1 Anteroposterior (AP) (A) and lateral (B) images of a patient after an endoscopic ALIF performed with paired threaded fusion cages and a posterior TLFS placement using cannulated screws. The most common contraindications include insufficient bone stock or excessive spinal instability. TLFSs rely on adequate purchase to the laminae, facets, and transverse processes. Marked osteopenia, lamina fracture, or excessive bone removal during decompression render the screws mechanically ineffective and are thus contraindications to their placement. At this point, safety and efficacy data for TLFS are available for limited indications. In that each segment is immobilized individually, and there are no intersegmental connections, their effectiveness in fusions greater than two levels remains to be demonstrated. In patients with significant instability or those who require reduction maneuvers, these implants are not indicated. For example, used alone, TLFSs do not provide adequate fixation in patients with isthmic or lytic spondylolisthesis, scoliosis, or in those with marked segmental kyphosis. TLFSs should not be used as stand-alone fixation in patients undergoing extension of a previous lumbar fusion. With experience, these screws are easy to place safely and quickly. However, careful attention to operative technique leads to more satisfactory outcomes. Limit the midline exposure to protect the paraspinal muscles. In the exposed region, clear off the lamina in its entirety to delineate its superior and inferior extent. Particularly if a decompression is to be performed, close assessment of the bone available will assist in planning both the decompression and subsequent TLFS placement. Similarly, remove the entire facet capsule and resect facet osteophytes. Denude the facet cartilage while protecting the subchondral bone. This enables clear identification of the drill as it passes in a biomechanically favorable perpendicular direction through the center of the facets joint. General anesthesia is used for most cases. In some cases, particularly when no posterolateral fusion is intended, spinal anesthesia may be recommended. Careful attention to positioning is critical. Failure to note hip flexion contractures and appropriate lordosis when positioning on the table may produce iatrogenic flatback deformity. TLFSs cannot be used in patients who require formal reduction maneuvers. On the other hand, some spinal flexion or extension may be introduced by compressing or distracting the spinous processes during drill passage. An oscillating drill has been recommended to decrease the possibility of wrapping up soft tissues. When placing the first screw, remember that another screw will be placed and space the entry point accordingly. That is, the first screw may have to be slightly more cranial than ideal and the second slightly more caudal. Because facet screws are placed essentially under direct vision, advanced imaging modalities are not required. Several manufacturers sell special guides for TLFS drill passage (Fig. 39.2). Most surgeons use these guides only for their first few cases and employ a “freehand” technique thereafter. Some surgeons place a feeler under the lamina during drill passage to act as a proprioceptive guide. Others have placed cannulated screws after drilling and tapping over a guide.
Facet Screw Placement
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








