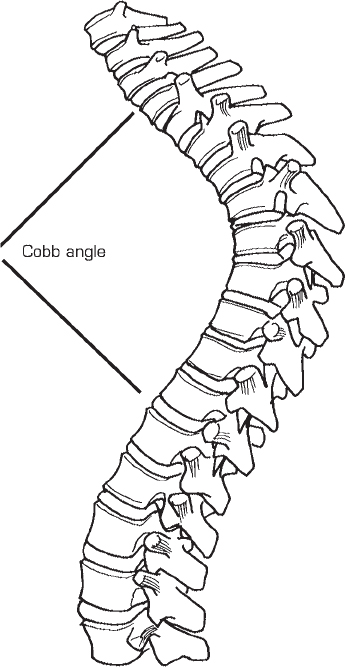
59 Kirkham B. Wood To safely and effectively stabilize the hyperkyphotic thoracic or thoracolumbar spine with bilateral rigid posterior segmental instrumentation while reducing the sagittal curvature into a more physiologic range. By first securing the longitudinal members (rods) proximally into multiple hook or pedicle screw anchors, careful judicious cantilever bending is used to deliver the rods into increasingly caudad sites of fixation and the hyperkyphosis is reduced. Modern instrumentation systems with their multiple sites of fixation and increased rigidity over those from previous eras allow not only improved construct rigidity and a higher rate of fusion, but also an ability to safely and consistently correct hyperkyphosis toward a more physiologic sagittal contour and to maintain that correction over time. Thoracic or thoracolumbar hyperkyphosis. Hooks (pedicle, transverse process, or laminar) have been historically the principal means of fixation. Although the transverse processes of the upper thoracic spine are potential sites of hook fixation, those of T10–T12 are frequently insufficient for adequate purchase, dictating the use of the laminae or pedicle screws for fixation. Pedicle screws, however, are increasingly recommended as anchors because of their increased pullout strength. Screws may also be used in all levels; however, the risk of a pedicle breach or neurologic injury should always be considered. The patient is positioned prone on either a four-poster frame or transverse rolls under the chest and pelvis. The operating table may be flexed slightly initially in severe cases, so that returning to the horizontal position aids in the reduction maneuver. Individuals with long-standing spinal deformity are often more osteopenic than control populations; thus, undue force should not be used to avoid fracture of the laminae or transverse processes if hooks are used. Pedicle screw fixation is strongly recommended in these situations. Because of the risk of proximal or distal fixation cutout during the reduction maneuver, especially in the elderly, wires can be passed around and through the end spinous processes or around the laminae, further securing the instrumentation. Additionally, a supra- or infralaminar hook at the ends of the constructs helps protect against pullout of the end pedicle screws. Posterior fusion alone typically works well, but in kyphosis surgery the incidence of pseudarthrosis is greatly affected by the degree of deformity. Hence, curves over 70 or 75 degrees usually require concomitant anterior fusion. In the event of insufficient posterior elements for hook fixation in the middle to upper thoracic region, pedicle screws should be used. Because of altered anatomy, intraoperative lateral radiographs or even C-arm imaging is strongly recommended to aid in the successful placement of pedicle screws. Care must be taken when performing this technique for shorter segment fixation situations such as thoracolumbar fractures. Often, after reducing the malalignment from the posterior approach, a significant “gap” may exist anteriorly from the deficient anterior column. A secondary anterior procedure to restore the column’s integrity may well be necessary. The major complication following the reduction of thoracic kyphosis is the development of a junctional kyphosis beyond the levels of instrumentation. Reasons for this include failing to include all kyphotic vertebrae proximally as well as distally including the first lumbar lordotic segment. Overcorrection of the kyphosis (>60%) is also associated with increased risk of proximal deformity. Careful preoperative hyperextension radiographs over a bolster will help define the spine’s rigidity and suggest expected degrees of correction. Age, osteopenia, and previous spine surgery should also be taken into consideration during the reduction maneuver as far as correction expectations are concerned. In cases of thoracic kyphosis (e.g., Scheuermann’s), the levels of posterior fusion and instrumentation should include the entire kyphosis as measured by the Cobb method to include the uppermost level of kyphosis down and including the first lordotic disk (often T12-L1) (Fig. 59.1). The basic instrumentation construct consists of a minimum of two claws, preferably three hooks or four to six pedicle screws on both sides above the apex of the kyphosis, and six to eight hooks or pedicle screws distally. Two 1/4-inch rods are bent to represent the desired kyphosis and then introduced first into the most proximal anchors and secured. Then, by careful cantilever bending, the rods are sequentially introduced into the more caudal hooks or screws (Fig. 59.2). Finally, segmental compression toward the apex of the kyphosis is applied.
Fixation Strategies and Rod Reduction Strategies for Sagittal Plane Deformities
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







