72
Halo Orthosis Application
Kenneth C. Moghadam and R. John Hurlbert
Description
Proper halo application creates long-term immobilization of the cervical spine while ensuring patient safety and comfort.
Key Principles
- Proper positioning of ring and screws
- Appropriate tightening of screws
- Snug-fitting vest
- Pin-site maintenance
Expectations
Effective halo application and care should confer immobilization for complex unstable cervical spine conditions without producing pain, difficulty swallowing, or visual obscuration, while at the same time allowing patient mobility.
Indications
For the nonsurgical management of cervical spine instability secondary to trauma, degenerative disease, infection, or as an adjunct to surgical reconstruction.
Contraindications
- Frontal, temporal, or parietal skull fractures
- Scalp laceration at pin site
- Head injury necessitating craniotomy
- Major chest injury
- Life-threatening abdominal injury
- Pulmonary insufficiency
Special Considerations
Skull pins should be retightened to 8 ft-lb at 24 to 36 hours postapplication. All other screws and straps should be checked and tensioned to their initial settings. The skin is cleansed in a circular fashion around each pin on a daily basis, utilizing sterilized cotton swabs soaked in normal saline. If crusts form on the skin at the pin sites, they should be moistened but not forcibly removed so as to prevent further skin breakdown. Mild irritation of the skin at the skull pins’ site is common. However, reddened, shiny, elevated skin with purulent discharge indicates local infection. Cultures should be obtained and topical antibiotics applied in conjunction with oral antibiotics. Relocation of a pin at an infected site may be necessary if the infection persists or if the torque setting cannot be maintained at a minimum of 6 in-lb.
A well-fitted vest is essential to maintain spinal alignment. Follow-up visitation is required to ensure pin site health, vest position, and wear as well as patient compliance. Typically at the terminus of care, which may be 12 weeks or longer in duration, radiographic evidence is obtained to determine fusion of the affected region. The positioning rods may be removed to allow for flexion and extension films without removing the ring.
Removal of the halo is most easily accomplished with the patient sitting in a chair. The lock nuts securing the skull pins should be loosened first. If spinal integrity or muscle weakness is a concern, a cervical collar may be applied prior to halo ring and vest removal. To disassemble the vest, the rods are removed first and then the chest and shoulder straps loosened on one side. The patient leans forward slightly so that both vest plates can be removed in one step. After loosening the locking nuts, the anterior skull pins are loosened and backed away from the skin to at least 1 cm of clearance. An assistant may hold the ring firmly from behind the patient to reduce migration as the posterior pins are removed. It is important before removing the ring to ensure that all pins are backed away with sufficient clearance to prevent laceration to the skin. An antibiotic ointment is applied to reduce bone exposure to air at the pin sites. The antibiotic is reapplied 24 hours later. Normal skin closure occurs within 36 hours. Patients should avoid washing their hair until this time.
For cardiac emergencies, halo manufacturers either create a pre-creased area on the anterior vest to facilitate access to the chest for compression or electrostimulation, or they supply a box wrench to loosen the anterior rods allowing access to the chest. After the emergency, the vest may be reapplied, refastened, or replaced according to the manufacturer’s specifications.
Special Instructions, Position, and Anesthesia
The superstructure allowing connection to the halo ring is applied to both the anterior and posterior vest plates, composed of support rods and connectors. The anterior vest is applied to the anterior chest wall and secured to the halo ring. The patient is gently log rolled to one side using spinal precautions, and the posterior vest is slid into position. The patient is returned to a supine attitude, and the posterior vest is fastened to the ring with the remaining rods and connectors. Vest straps are applied to firm tension at the abdomen and shoulders. It may be necessary to reposition the head for best spinal alignment. Typically a neutral position is best; it is seen as an imaginary vertical line from the inferior lobe of the ear to the inferior tip of the nose. Radiographic evidence is required to confirm cervical alignment.
Positioning of the vest may require special attention in certain circumstances. Morbidly obese patients may require special accommodation of vest size and positioning, as it is important to ensure that the distal border of the anterior vest is superior to the diaphragm, leaving sufficient space for abdominal expansion for respirations. Emaciated patients require attention to potential pressure points to reduce risk of skin ulceration.
Tips, Pearls, and Lessons Learned
Surgical bed adapters are commercially available to allow fixation of the halo ring to the operating table. Once positioned on the table and fixed in the adapter, the anterior or posterior vest may be removed easily without compromise to the cervical spinal alignment. If necessary, reapplication postoperatively is easily accomplished, with the adapter maintaining the head position.
Imaging
Most halo orthoses are magnetic resonance imaging (MRI) compatible; however, the manufacturer’s specifications should be examined to ensure compliance.
Pediatric Applications
Selection of an appropriately sized ring is important. Measure the circumference of the head 1 cm above the ear and eyebrows and select the appropriate ring according to the halo manufacturer’s sizing chart. In general, a closed ring is preferred to an open ring to accommodate the greater number of pin sites necessary due to immature development of the cranium. The number of pins placed into the skull and the degree to which they are tightened are age specific (Table 72.1).
| Patient Age | Number of Pins | Torque (in-lb) |
| <5 | 8–12 | 2–3 |
| 6–14 | 6–8 | 4–6 |
| 15–17 | 4–6 | 6–8 |
| Adult | 4 | 8 |
Key Procedural Steps
Ring Type and Size
Halo rings are available in two styles, open-backed (horseshoe shaped) and closed-backed (ring shaped). The open-backed ring simplifies application because the patient’s head can remain flat on the bed during positioning and pin insertion. It also leaves the posterior neck and occiput well exposed if posterior surgical management is required. The closed-backed ring allows for a greater number of pin placements. Different manufacturers provide rings of different sizes. A properly fitting ring should allow for about 1 to 2 cm of clearance circumferentially from the scalp, when positioned at or just below the equator of the skull.
Ring Application
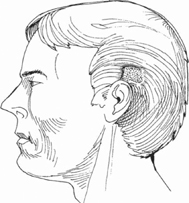
The patient is positioned supine on the hospital bed. A positioning plate called a “spoon” is inserted underneath the patient in the midline of the spine so that it spans from the inferior border of the scapula to the posterior pole of the occiput. While gentle in-line traction is maintained, the patient and spoon are drawn up the bed to allow the head and neck to rest on the spoon, extending freely off the top of the bed. It is necessary to shave a 2.5-cm 2 area just behind and above the ear in preparation for the posterior (parietal) pins (Fig. 72.1). The frontal and parietal pin sites are prepared with Betadine, chlorhexidine, or alcohol sterilization.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







