37
Lumbar Pedicle Screw Placement
Robert W. Molinari
Description
To accurately place screws through the pedicles of the lumbar vertebrae with particular attention given to the avoidance of intraoperative and postoperative complications.
Key Principles
Pedicles are short conical tubes with an oval cross section. The objective is to place the screws through the center of the pedicles and into the vertebral body. The screws should converge toward the midline to ensure that they do not penetrate the lateral wall of the vertebral body. Segmental instrumentation systems using lumbar pedicle screws are extremely effective in restoring and maintaining normal sagittal and coronal spinal alignment.
Expectations
The goals of lumbosacral segmental instrumentation are to reduce deformity (such as that seen in scoliosis, spondylolisthesis, kyphosis, and trauma) and to provide stability. The pedicle is the strongest portion of the vertebra. Screws placed into the pedicles may provide rigid three-column fixation of the lumbar spine. Increasing construct rigidity enhances the chance for successful fusion and maintained spinal alignment.
Indications
- Spondylolisthesis reduction
- Degenerative spondylolisthesis fusion
- Instability as a result of trauma or tumors
- Wide, destabilizing decompression
- Stabilization after osteotomy
- Posterior stabilization of degenerative disks
- Scoliosis correction and stabilization
Contraindications
- Severe osteopenia
- Inadequate pedicle size or morphology
- Fractured or diseased pedicle
Special Considerations
Patients with severe osteoporosis may not be suitable for lumbar pedicle screws. Bone density less than 0.45 g/cm2 has been associated with pedicle screw loosening. Insertional torque will demonstrate the screw’s degree of purchase in the bone. Undertapping, no tapping, and use of conical screws have been demonstrated to improve screw pullout strength. Approximately 75% of screw purchase is obtained in the pedicle. The screw should cross the midportion of the vertebral body in the lateral plane. Typically, 6-mm-diameter and 40- to 45-mm length screws are used. Screws that violate the anterior cortex of the vertebral body are not recommended due to the increased risk of vascular injury.
Special Instructions, Position, and Anesthesia
A radiolucent table is imperative for proper anteroposterior (AP) and lateral intraoperative imaging during screw placement. Positioning the hips in extension improves lumbar lordosis. Fusing multiple segments of the lumbar spine with the hips positioned in flexion may cause iatrogenic flatback deformity. General anesthesia is used in patients for lumbar pedicle screw instrumentation.
Tips, Pearls, and Lessons Learned
Appropriate positioning of the transpedicular screws in the lumbar spine is dependent on proper visualization of the posterior anatomic landmarks for insertion. Knowledge of the anatomy of the pedicle in relation to the neural structures is crucial. The nerve root is situated just medial and inferior to the pedicle as it exits into the intervertebral foramen. Violation of the pedicle cortex in this area may cause injury to the exiting nerve root.
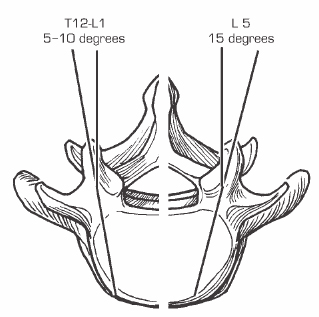
The entry point for the pedicle is at the intersection of a vertical line tangential to the lateral border of the superior articular process and a horizontal line passing through the middle of the insertion of the transverse process, or 1 mm below the joint line. The screws should be angled approximately 5 degrees medially at L1, 10 degrees at L2, and increasing to 15 degrees at L5 (Fig. 37.1). The amount of medial angulation of the pedicle varies depending on the level and on the surgeon’s entry point location. Lateral entry points on the transverse process require greater medial angulation. Medially placed entry points on the superior facet may not require any medial angulation. Preoperative imaging studies should be used to determine the exact angulation, depth, and size of the pedicle. Intraoperative AP fluoroscopy will reliably identify the starting point’s relation to the pedicle walls.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








