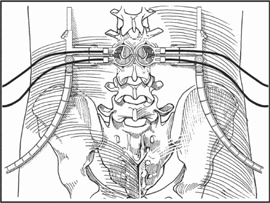
65 James D. Schwender, Kevin T. Foley, and Langston T. Holly Minimally invasive techniques have revolutionized the management of pathologic conditions in various surgical disciplines. The objective is to reduce the approach-related morbidity and at the same time allow the surgery to be performed in an effective and safe manner. The systems currently available consist of a series of concentric dilators and thin-walled tubular retractors of variable length. The tube circumferentially defines a surgical corridor through the erector spinae muscles. This technique is appropriate for the surgical treatment of lumbar disk herniation, spinal stenosis, or in cases that require stabilization. The current retractor systems are designed to allow exposure of one and two lumbar levels. In the case of stenosis, ipsilateral and contralateral decompression of central, subarticular, and foraminal stenosis is possible through a single paramedian incision. Published outcomes for decompression surgery compare favorably to the traditional midline open technique. Same-day surgery has become the rule. Concerning one- and two-level fusions, in experienced hands, the blood loss and hospitalization are typically reduced by 50%. Outcomes again compare favorably to traditional techniques. Operative times and complication rates for both decompression and fusions are similar compared with open techniques. The indications are the same as the surgeon would use for tradition open procedures at one or two levels in the lumbar spine for either decompression or fusion. Relative contraindications currently include the following: Knowledge of three-dimensional spinal anatomy is fundamental in the mastery of less invasive techniques. Not infrequently, the surgeon relies on live or virtual fluoroscopic images displayed on a monitor or threedimensional images from an image guidance system for anatomic orientation. This can be challenging for surgeons who have not had significant experience using two-dimensional images to determine their three-dimensional surgical position. Patient positioning and good intraoperative imaging are essential. It is also important to choose the correct size retractor for the given procedure. For decompression, a smaller diameter retractor is required to allow placement medial to the facet joint. This minimizes the amount of soft tissue creep into the wound. The same holds true for fusions. In this case, a larger diameter retractor is docked over the facet joint to be fused again to prevent muscle creep. This allows for identification of the anatomy for decompression and fusion. Once the retractor is in the correct position, resist the temptation of moving the retractor often, which leads to creep of the muscle into the wound. The treatment of an incidental durotomy should proceed in a similar fashion as if this complication was encountered in an open procedure. A primary suture repair is preferable if it is possible. If a watertight repair cannot be achieved, TisseelTM (Baxter, Deerfield, IL), DuraGenTM (Integra Life Sciences Corp., Plainsboro, NJ), or other dural repair products are useful. In our experience, the minimal dead-space created by the less invasive procedures seems to limit the formation of a symptomatic pseudomeningocele. The working retractor size for decompression varies between 12 and 18 mm and for fusions between 22 or 26 mm. The patient is positioned prone on a Jackson or Wilson frame to allow a C-arm fluoroscope to be used in a biplanar fashion. It is important to confirm that both views are technically possible and the anatomy of the spine is well visualized prior to prepping and draping. The position of the skin incision is determined based on the pathology to be addressed and is localized using the orthogonal fluoroscopic images. Typically, the incision is 2 to 3 cm off midline for disk herniations and stenosis that require assessment through the interlaminar space and 4 to 5 cm for foraminal herniations, TLIF, or posterolateral fusion (Fig. 65.1).
Minimally Invasive Posterior Surgical Approaches to the Lumbar Spine Through Tubular Retractors
Description
Expectations
Indications
Contraindications
Special Considerations
Tips, Pearls, and Lessons Learned
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







