6
Occipital Wiring and Plating Techniques
Neal G. Haynes, Troy D. Gust, and Paul M. Arnold
Description
The safe fixation of the occipital cervical junction with both plates and screws, or wires, cables, and rods, without durotomy, neural, or vascular injury. Internal occipital-cervical stabilization has proven over time to be advantageous to external fixation for complication-free immobilization of the unstable occipital cervical junction.
Expectations
Occipital screws and plates are more stable under axial loads and should be considered for severe instability or when needed to counterbalance additional force vectors such as odontoid migration or multiple fractures.
Wires secured to the inner surface of the occipital bone can provide a solid point of purchase to secure cervical rods. This avoids potential screw pullout and can be used when bone is less than optimal. Additionally, this provides flexibility to the surgeon in choosing cervical wire purchase location.
Indications
Occipitocervical instability or dislocation from trauma, rheumatoid arthritis or other inflammatory process, basilar impression, neoplasm, congenital anomalies, osteomyelitis, or iatrogenic causes.
Contraindications
Active infection, irreducible odontoid migration greater than 15 mm above the foramen magnum, or presence of a sequestrum.
Special Considerations
Preoperative planning should include computed tomography (CT) scanning to locate the transverse sinus as well as any anomalous vasculature to prevent inadvertent vascular injury. Preoperative positioning with lateral x-ray or fluoroscopic guidance is crucial to establish optimal alignment of the basiocciput and cervical spine to prevent postoperative occipitocervical kyphosis. The patient is placed in the prone position secured in a Mayfield head holder. In cases of spinal cord compression, somatosensory or motor evoked potential monitoring should be used.
Tips, Pearls, and Lessons Learned
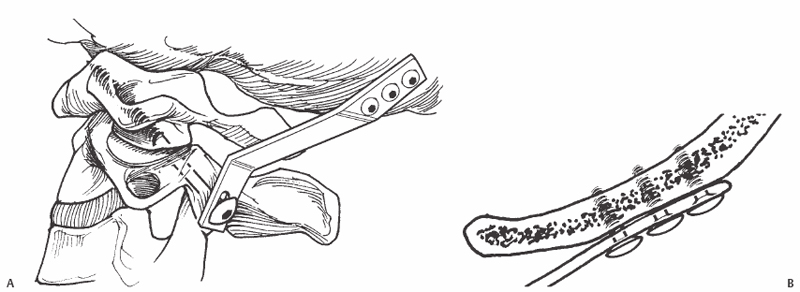
For dual plating, occipital screws should be placed three to a side on either side of the midline just below the superior nuchal line and as close to the external occipital protuberance as possible (Fig. 6.1). An independent occipital plate may only require two or three screws, usually oriented in a vertical or transverse orientation. Cerebrospinal fluid (CSF) leaks at this stage can usually be stopped by placing a screw into the hole. Bone wax may also be helpful to prevent CSF leak.

Fig. 6.1 Upper cervical spine and occiput. Note there are three holes on each side for the cranial fixation.
For wire placement, intraoperative fluoroscopy is useful in that it helps to match the malleable rod template to the profile of the occipitocervical junction. The rod implant is then bent to match the template. Patience is required during this step to ensure that the rods rest on the occiput and that no space exists between the rods and the cervical lamina, as this can result in the wire cutting through the bone. A small suboccipital craniotomy surrounded by four burr holes can make wire passage easier and safer. Bending the tip of the wire 180 degrees over a distance of less than 10 mm such that the bend is being advanced between the bone and dura rather than the blunt end can help prevent inadvertent durotomy and neural injury.
Key Procedural Steps
Occipital screw placement immediately lateral to the external occipital protuberance and up to 20 mm laterally along the superior nuchal line can accommodate screws from 14 mm in length medially to 5 mm in length at 20 mm. This optimal screw placement zone tapers downward to the foramen magnum in a triangular fashion. Bicortical occipital fixation provides the strongest construct. To do this, both the inner and outer table must be drilled and tapped prior to screw placement. Before drilling, the drill stop should be set to 10 mm.
C2 pedicle screws should be placed first, followed by subaxial lateral mass screws. Occipital screws may be placed after cervical fixation, as there is more room for variability at the occiput than in the spine (Fig. 6.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








