30
Open Transthoracic Diskectomy
Russel C. Huang, Patrick F. O’Leary, and Raja Taunk
Description
Open transthoracic diskectomy is performed to decompress symptomatic thoracic herniated nucleus pulposus (HNP) in patients with myelopathy or myeloradiculopathy.
Key Principles
The reported radiographic prevalence of thoracic herniated disks in asymptomatic individuals is 37%. Therefore, radiographic findings must be well correlated with the history and physical examination findings before recommending surgery. Neural compression may result in myelopathy or radiculopathy. Myelopathy may manifest as motor, sensory, or reflex changes distal to the level of compression, gait disturbance, and bowel/bladder dysfunction. Radiculopathy may result in pain or sensory changes in a dermatomal distribution. The differential diagnosis includes cervical or lumbar stenosis, herpes zoster, infections or neoplasms, central nervous system disorders, and systemic or peripheral neuropathies. Thoracic axial pain from disk disease should be treated nonsurgically in most cases.
Selection of anterior or posterior approaches for thoracic decompression hinges upon the location and character of the herniation. Most authors agree that the transthoracic approach offers superior visualization of the disk and dura in the central zone of the spinal canal. Although lateral disk herniations can safely be decompressed via anterior or posterior approaches, the surgical morbidity of posterior approaches is lower than that of thoracotomy.
Expectations
Surgery is performed to prevent progressive neurologic injury from ongoing cord compression. Despite adequate decompression, preexisting neurologic deficits may not resolve. Thoracic axial pain may not improve. The risk of postoperative paralysis is significantly higher than the risk of paralysis after cervical or lumbar decompressive surgery.
Indications
- Absolute: Myelopathy with progressive neurologic deficits
- Relative: Painful radiculopathy from a thoracic HNP not amenable to posterior decompression
Contraindications
Pulmonary disease prohibiting safe thoracotomy.
Special Considerations
Preoperative Planning
In addition to standard imaging, it is useful to obtain a continuous computed tomography (CT) or magnetic resonance imaging (MRI) scan that includes the entire thoracic and lumbosacral spine. The scans should be correlated with plain films and scrutinized for supernumerary vertebrae, rib abnormalities, or lumbosacral transitional anomalies that might generate confusion in the intraoperative identification of levels.
Measure the mediolateral width of the vertebral body at the level of the ventral floor of the spinal canal using CT or MRI. Knowing this width is helpful in ensuring that the mediolateral extent of disk removal is adequate.
Tips, Pearls, and Lessons Learned
- We recommend intraoperative neural monitoring.
- Extensive calcification of the disk appears to raise the risk of intraoperative dural tears.
- A beanbag is useful to maintain true lateral decubitus positioning intraoperatively.
- Maintaining the patient in true lateral position keeps the surgeon oriented to the spinal canal and spinal cord.
- The rib, as the embryologic equivalent of the lumbar transverse process, leads to the identically numbered pedicle (e.g., tenth rib to T10 pedicle)
- Hypotensive anesthesia is not desirable. Blood pressure should be maintained normo- to hypertensive to maintain cord perfusion.
Key Procedural Steps
The patient is placed in the lateral decubitus position. Above T6 a right-sided approach is preferred to avoid the heart and aortic arch. Below T6, left-sided approaches are preferred because the aorta is relatively safer to handle and mobilize. The break in the table is positioned at the level of interest and aids in exposure. The chest is usually entered one or two rib levels above the disk of interest. After entering the chest cavity, the ipsilateral lung is deflated using a double-lumen endotracheal tube. Preliminary identification of levels may be aided by intrathoracic palpation of the first rib and counting distally. Intraoperative radiographs are taken to confirm levels. In most cases, visualization of the 12th rib and corresponding vertebral body on anteroposterior radiographs provides the most reliable identification of levels.
Once the appropriate level has been identified, the rib head overlying the disk is resected. The neurovascular bundle caudal to the rib should be identified and protected. If necessary, the segmental artery should be ligated as distant from the foramen as possible to best preserve cord perfusion. Following rib head removal, dissecting and tracing the neurovascular bundle medially leads to the foramen, the pedicle, and the lateral margin of the disk and vertebral bodies.
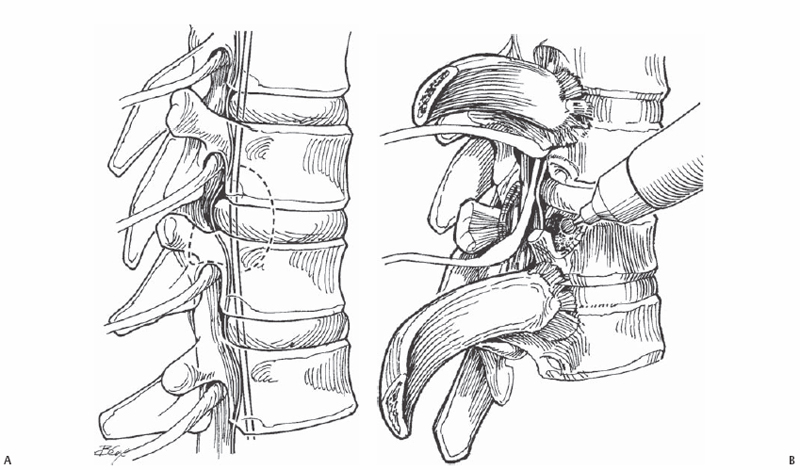
The caudad pedicle is thinned with a burr and resected with a Kerrison rongeur, revealing the lateral aspect of the dural tube (ventral margin) of the spinal canal, and the disk itself (Fig. 30.1). Do not attempt to place any instruments between the disk and the cord at this time. A burr is used to perform partial corpectomies above and below the affected disk, leaving undisturbed the posterior shell of bone and disk material that is in direct contact with the dura (Fig. 30.2). Preoperative measurement of the width of the vertebral body is helpful in determining how “deep” to go with the burr to reach the other side of the spinal canal (right side of the canal in a left-sided approach).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








