79
Posterior Revision Strategies for Dura and Nerve Root Exposure Following a Previous Laminectomy
Erik Spayde and Hyun Bae
Description
Revision decompression surgery is a challenging aspect of spinal surgery that may be facilitated by following a routine set of surgical guidelines and operative techniques. A thorough preoperative evaluation of a patient contemplating revision spine surgery is essential to minimize complications, increase operative efficiency, and ensure the best possible outcome for the patient.
Expectations
Appropriate levels for revision decompression should be determined based on a patient’s history, physical exam, and radiographic data. Preoperative planning includes an understanding of a patient’s original symptomatology prior to the initial surgical procedure, review of all historical and recent imaging studies, and a detailed informed consent reviewing realistic expectations following a revision procedure. Blood loss, operative time, and outcomes are usually less predictable than the index procedure. Informed consent may include the possibility that preoperative neurologic deficits may be permanent and not improved with surgery. Patients should also be informed of the potential need for bed rest and for flat head of bed positioning for 48 to 72 hours postoperatively in the event of a dural injury.
Indications
The most common indication is recurrent symptoms of radiculopathy from a previously decompressed lumbar segment. Causation can be associated with new onset or progressive instability, recurrent disk herniation, facet hypertrophy causing lateral recess stenosis, reoccurring facet cyst, adjacent level stenosis, and an incomplete primary decompression.
Contraindications
An absolute contraindication does not exist, but some situations should be recognized as challenging, requiring the preparation of different treatment options or possibly a different approach altogether. For instance, in the case of a recurrent disk herniation or a lateral disk herniation in which the remaining pars may have to be sacrificed, an easier and safer approach would be to plan for a transverse lateral decompression and an interbody fusion. The decompression could then be performed lateral to medial, sacrificing the pars and allowing for a complete and thorough decompression. An even more challenging scenario is a recurrent disk at the level that a conjoined nerve root was identified from a previous decompression. In this case any root retraction would be extremely difficult and may cause injury to the root itself. This case is best probably approached with an anterior diskectomy and decompression, thus avoiding the posterior approach altogether.
Special Considerations
Obtaining previous patient charts is an important diagnostic tool. Past records may reveal important information about the patient’s symptoms on initial presentation, previous operation, and response to treatment. Long-standing symptoms that were unimproved with appropriate surgical treatment may indicate that permanent neurologic deficits are present. Conversely, inadequate initial decompression with persistent symptoms may portend a favorable outcome to revision surgery. Timing of the previous surgery is also a critical factor to consider. Previous surgery within 2 to 3 weeks may not exhibit the same scar formation and adhesions of more distant surgeries. Decompressions performed over 1 year previously may be complicated not only by abundant scar adhesions but also by lateral recess bone regrowth and advanced facet degeneration.
Plain radiographs should be a routine component of the initial radiographic workup. Standing antero-posterior, lateral, and flexion-extension views are useful in evaluating the extent of the previous decompression, degenerative changes, instability, and other pathology such as tumor or infection. Previous decompression procedures may result in unstable spondylolisthesis or spondylolysis, which may be elucidated on flexion-extension or oblique radiographs or advanced imaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI). MRI may be performed with and without gadolinium to aid in differentiating scar from other pathologies. MRI is also helpful in identifying the presence of a pseu-domeningocele and arachnoiditis. Pseudomeningocele may sometimes be confused with a seroma. Arachnoiditis typically appears as irregular nerve roots that are thickened or clumped together. MRI may have limited utility, however, due to excessive postoperative scar formation or the presence of metal instrumentation, which produces artifact. The mainstay of postoperative imaging is postmyelography CT.
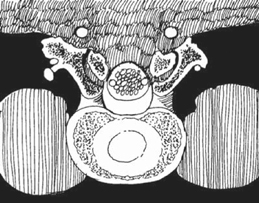
A CT myelogram is useful in evaluating the bony anatomy. Pars interarticularis defects may easily be identified as well as the presence of bridging laminar bone that may still be present if the previous procedure was a limited type of decompression. These bony structures serve as important landmarks. Another crucial observation is the level of the pars with respect to the dura. With the exception of L5-S1, the pars is usually posterior to the most superficial portion of the dura, making this a critical landmark for safely resecting epidural scar tissue (Fig. 79.1). At L5-S1 the dura is often above the level of the pars, however, and scar resection must be carefully performed at this level to avoid an inadvertent durotomy. Pseudomeningocele identified on MRI is also important to confirm on CT myelogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








