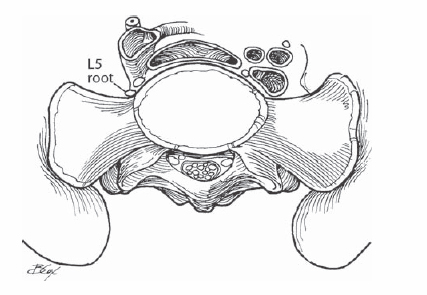
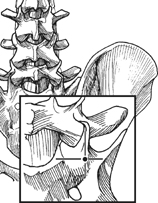
43 Daniel E. Gelb Mechanical stabilization of the distal lumbar spine to the pelvis (lumbosacral joint) may be achieved with the use of screws inserted into the proximal sacrum incorporated into mechanical constructs that span the lumbosacral joint. This method of fixation is widely adaptable, more rigid than hook-based constructs, and more effectively maintains anatomic alignment (lordosis). Pedicle screw-based segmental fixation systems provide rigid fixation with control of all three columns of the spine. However, anatomic considerations limit options for screw placement because placement of screws outside the anatomic boundaries of the pedicle may result in iatrogenic neurovascular injury. The sacral spinal canal contains the distal elements of the cauda equina (S1 to S5). The iliac vessels lie immediately anterior to the lumbosacral disk, whereas the L5 nerve root lies anterior to the ala of the sacrum, medial to the sacroiliac joint (Fig. 43.1). Although the S1 pedicle is broad, the bone density of the proximal sacrum is poor. This deficiency necessitates bicortical purchase of S1 screws to ensure optimal screw purchase and may require supplemental fixation techniques to obtain adequate mechanical stability. Fig. 43.1 The common iliac vessels and L5 nerve roots travel immediately anterior to the lumbosacral disk and S1 body lateral to the midline, making bicortical screw fixation possible. Adequate surgical exposure and thorough understanding of sacral pelvic anatomy allows safe placement of screws within the sacrum. Medially directed bicortical S1 screws are the preferred technique. Laterally directed screws into the sacral ala can be used as an adjunct or as a substitute for medially directed screws when standard implantation is unfeasible. S2 pedicle screws are used to supplement proximal sacral fixation sites for enhanced mechanical stability. Medially directed S1 pedicle screws are the preferred technique. Large-diameter S1 pedicles and poor bone quality in the body of S1 make bicortical screw insertion a more rigid option than unicortical fixation. Anterior cortical penetration may put the viscera, iliac vessels, or L5 nerve root at risk. Graduated punches with stops are available to safely perforate the anterior sacral cortex and measure appropriate screw length. Screws should penetrate the anterior cortex medial to the iliac vessels. Screws should be placed parallel to the superior sacral end plate or toward the promontory. In muscular patients with a narrow pelvis, it may be difficult to achieve the appropriate angulation to the midline. Retraction of the paraspinal muscles is blocked by the iliac wings. The patient is positioned prone on a spinal frame with care taken to avoid pressure on the abdomen. General anesthesia is employed. Hips should be placed in maximal extension to enhance lumbar lordosis and prevent iatrogenic postoperative flatback syndrome. The sacral pedicle is large, and use of a large-diameter (7-mm) screw is generally necessary to obtain adequate pedicle fill. Adequate exposure of the sacral ala may be difficult. Brisk bleeding may occur lateral to the superior sacral facet in the depth of the lateral gutter. Lumbosacral lordosis may require extreme rod contouring. A high rate of failure of stand-alone S1 pedicle screws has been reported in long constructs. Consideration should be given to supplementary pelvic fixation anchor points or rigid structural anterior column support to protect the S1 screws in these situations. Adequate exposure of the correct starting point may be difficult in heavyset muscular patients. A narrow pelvis with tall posterior iliac wings may prevent appropriate medial screw trajectory. Exposure of the posterior elements of the lumbosacral junction is completed through either a midline or paramedian approach. In particular, the soft tissues adjacent to the lumbosacral facets and ala must be stripped for adequate visualization of bony landmarks. The starting point for the medially directed S1 screw is the confluence of the base of the superior sacral facet and the ala of the sacrum (Fig. 43.2). The posterior cortex is opened with either a burr or an awl. A blunt pedicle probe or curette is passed through the sacral pedicle perpendicular to the posterior sacral cortex aiming 20 to 30 degrees medially (Fig. 43.3). Directing the probe in a slightly more vertical orientation allows the tip of the screw to abut the superior end plate of the sacrum or into the promontory, the area of greatest bone density (Fig. 43.4).
Sacral Screw Fixation Techniques
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







