Chapter 5 Stupor and Coma
Definitions
Consciousness may be defined as a state of awareness of self and surroundings. Alterations in consciousness are conceptualized into two types. The first type affects arousal and is the subject of this chapter. The second type involves cognitive and affective mental function, sometimes referred to as the “content” of mental function. Examples of the latter type of alteration in consciousness are dementia (see Chapter 6), delusions, confusion, and inattention (see Chapter 9). These altered states of consciousness, with the exception of advanced dementia, do not affect the level of arousal. Sleep, the only normal form of altered consciousness, is discussed in Chapter 68.
Conditions That May Mimic Coma
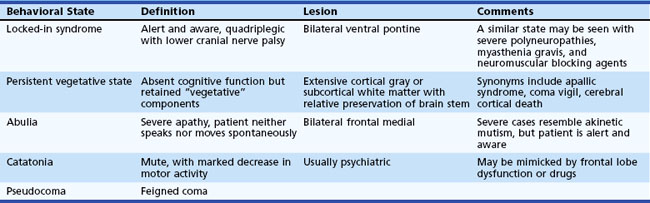
Several different states of impaired cognition or consciousness may appear similar to coma or be confused with it (Table 5.1). Moreover, patients who survive the initial coma may progress to certain of these syndromes after varying lengths of time. Once sleep/wake cycles become established, true coma is no longer present. Differentiation of these states from true coma is important to allow administration of appropriate therapy and help determine prognosis.
In the persistent vegetative state (PVS), patients have lost cognitive neurological function but retain vegetative or noncognitive neurological function such as cardiac action, respiration, and maintenance of blood pressure. This state follows coma and is characterized by absence of cognitive function or awareness of the environment despite a preserved sleep/wake cycle. Spontaneous movements may occur, and the eyes may open in response to external stimuli, but the patient does not speak or obey commands. Diagnostic criteria for PVS are provided in Box 5.1. Diagnosis of this condition should be made cautiously and only after extended periods of observation. A number of poorly defined syndromes have been used synonymously with PVS, including apallic syndrome or state, akinetic mutism, coma vigil, alpha coma, neocortical death, and permanent unconsciousness. These terms, used variously by different authors, probably are best avoided because of their lack of precision.
Box 5.1
Criteria for Diagnosis of Persistent Vegetative State
1. No evidence of awareness of themselves or their environment; they are incapable of interacting with others
2. No evidence of sustained, reproducible, purposeful, or voluntary behavioral responses to visual, auditory, tactile, or noxious stimuli
3. No evidence of language comprehension or expression
4. Intermittent wakefulness manifested by the presence of sleep/wake cycles
5. Sufficiently preserved hypothalamic and brainstem autonomic functions to survive if given medical and nursing care
6. Bowel and bladder incontinence
7. Variably preserved cranial nerve (pupillary, oculocephalic, corneal, vestibulo-ocular, and gag) and spinal reflexes
Data from The Multi-Society Task Force on PVS, 1994. Medical aspects of the persistent vegetative state. N Engl J Med 330, 1499-1508, 1572-1579.
A condition that has been estimated to be 10 times more common than PVS is the minimally conscious state, in which severe disability accompanies minimal awareness. A set of diagnostic criteria for the minimally conscious state has been proposed (Box 5.2). Abulia is a severe apathy in which patients have blunting of feeling, drive, mentation, and behavior such that they neither speak nor move spontaneously.
Box 5.2
Criteria for the Minimally Conscious State
2. Gestural or verbal yes/no responses (regardless of accuracy)
4. Purposeful behavior, including movements or affective behaviors that occur in contingent relationship to relevant environmental stimuli and are not due to reflexive activity
Data from Giacino, J.T., Ashwal, S., Childs, N., et al., 2002. The minimally conscious state: definition and diagnostic criteria. Neurology 58, 349-353.
Approach to the Patient in Coma
The initial clinical approach to the patient in a state of stupor or coma is based on the principle that all alterations in arousal constitute acute life-threatening emergencies until vital functions such as blood pressure and oxygenation are stabilized, potentially reversible causes of coma are treated, and the underlying cause of the alteration in arousal is understood. Urgent steps may be necessary to avoid or minimize permanent brain damage from reversible causes. In view of the urgency of this situation, every physician should develop a diagnostic and therapeutic routine to use with a patient with an alteration in consciousness. A basic understanding of the mechanisms that lead to impairment in arousal is necessary to develop this routine. The anatomical and physiological bases for alterations in arousal are discussed in Chapter 68.
Although it is essential to keep in mind the concept of a spectrum of arousal, for the sake of simplicity and brevity only the term coma is used in the rest of this chapter. Table 5.2 lists many of the common causes of coma. More than half of all cases of coma are due to diffuse and metabolic brain dysfunction. In Plum and Posner’s landmark study (1980, see 2007 revision) of 500 patients initially diagnosed as having coma of unknown cause (in whom the diagnosis was ultimately established), 326 patients had diffuse and metabolic brain dysfunction. Almost half of these had drug poisonings. Of the remaining patients, 101 had supratentorial mass lesions, including 77 hemorrhagic lesions and 9 infarctions; 65 had subtentorial lesions, mainly brainstem infarctions; and 8 had psychiatric coma.
| I. SYMMETRICAL-NONSTRUCTURAL |
| Toxins |
| Drugs |
| II. SYMMETRICAL-STRUCTURAL |
| Supratentorial |
| III. ASYMMETRICAL-STRUCTURAL |
| Supratentorial |
| Metabolic |
| Subarachnoid Hemorrhage |
| Subdural Hemorrhage, Bilateral |
| Infections |
| Psychiatric |
| Catatonia |
| Other |
| Infratentorial |
| Subdural Empyema |
* Relatively common asymmetrical presentation.
Data from Plum, F., Posner, J.B., 1980. The Diagnosis of Stupor and Coma, third ed. F.A. Davis, Philadelphia; and from Fisher, C.M., 1969. The neurological examination of the comatose patient. Acta Neurol Scand 45, 1-56.
Rapid Initial Examination and Emergency Therapy
The risk of herniation from an LP in patients with evidence of increased intracerebral pressure is difficult to ascertain from the literature; estimates range from 1% to 12%, depending on the series (Posner et al., 2007). It is important to recognize that both central and tonsillar herniation may increase neck tone.
History
The neurologist often is called when patients do not awaken after surgery or when coma supervenes following a surgical procedure. Postoperative causes of coma include many of those listed in Table 5.4. In addition, the physician also must have a high index of suspicion for certain neurological conditions that occur in this setting, including fat embolism, addisonian crisis, hypothyroid coma (precipitated by acute illness or surgical stress), Wernicke encephalopathy from carbohydrate loading without adequate thiamine stores, and iatrogenic overdose of a narcotic analgesic.
Finally, family members or friends may be invaluable in identifying psychiatric causes of unresponsiveness. The family may describe a long history of psychiatric disease, previous similar episodes from which the patient recovered, current social stresses on the patient, or the patient’s unusual idiosyncratic response to stress. Special care must be taken with psychiatric patients because of the often biased approach to these patients, which may lead to incomplete evaluation. Psychiatric patients are subject to all the causes of coma listed in Table 5.4.
General Examination
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree