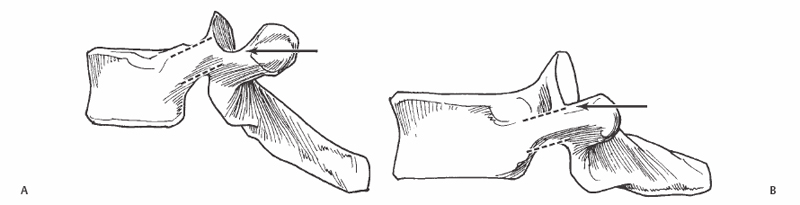
25 Kingsley R. Chin A technique that allows surgeons to “safely” access the intervertebral disk and lesions in the pedicle and vertebral body, and to decompress the neural elements through a posterior approach. The protective walls of the pedicles provide a safe pathway to access the pedicles, vertebral bodies, and intervertebral disks. This technique decreases the risks and potential morbidity that would be associated with costotransversectomy or an anterior thoracic approach for the same pathology. In cases of intrapedicular lesions, it is the technique of choice. Focal midline anterior spinal cord compression. Access to the pedicle without fluoroscopic assistance will necessitate either a laminotomy to probe the medial pedicle wall or resection of the proximal rib head or transverse process to access the lateral pedicle wall. Patients with a fusion mass and a laminectomy membrane may necessitate the use of fluoroscopy to access the pedicle. Patients with rotatory kyphoscoliosis may need a combination of fluoroscopy and direct palpation as described above to follow the pedicle trajectory for risk of breakthrough and injury to the displaced great vessels. Placing the patient in the prone position on a Jackson table to facilitate maneuverability of the fluoroscope is preferred, but the choice of position may be based on stabilization techniques and other factors. Motor and sensory evoked potential monitoring is preferred. A double-lumen tube is used to allow single lung ventilation if needed. General anesthesia is preferred, with or without supplementation with local long-acting anesthetic. Review the preoperative axial images to understand the pedicle anatomy and map the location of the pathology. Three-dimensional reconstruction is advised. To access the pedicle under direct vision, remove the rib head and transverse process, or perform a laminotomy. Removal of the lateral pedicle walls, transverse process, and rib head enables greater access to the midline. If uncomfortable localizing the pedicle visually, use a gearshift to localize and penetrate the pedicle under biplanar fluoroscopic guidance followed by a 4.2 tap to core out a path as you would for pedicle screw placement. The gearshift should not advance beyond 80% of the distance to the anterior cortex to avoid anterior cortical penetration. Frequent fluoros-copy is suggested to monitor the leading depth of penetration during decompression. Anterior column support may be improved with a concomitant transpedicular placement of autogenous bone graft or other osteobiologics. Excessive cancellous bleeding may occur. Use hemostatic aids liberally and work expeditiously. Medial wall breech may cause dural tear, neural injury, and excessive epidural bleeding, necessitating a laminotomy or laminectomy. Use of intraoperative ultrasound diminishes the risk of inadequate decompression of midline structures, although this is rarely necessary in practice. Fluoroscopy is used to localize the incision. A midline incision is used but only the ipsilateral erector spinae muscles are dissected free off the posterior elements unless bilateral transpedicular approaches are planned. The exposure should include the entire lamina, transverse process, and rib-head/costovertebral junction of the selected vertebra. Biplanar fluoroscopy can be used to localize the pedicle, which is situated directly inferior to the superior articular process and at the level of the top of the transverse process in the upper thoracic spine, but at the level of the middle to lower half of the transverse process in the lower thoracic spine (Fig. 25.1). The posterior cortex of the pedicle is opened with a high-speed burr. Sequentially larger curettes are used to develop the medullary canal of the pedicle down to the vertebral body. Sequential fluoroscopic views are used to assess the depth of decompression at intervals. Alternatively, a faster decompression can be achieved with a high-speed burr along a channel that was previously developed with a gear shift and tapped. Once the appropriate depth is reached and localized fluoroscopically, the transpedicular channel should allow passage of angled curettes at 45-degree angles to each other to remove bone through the opposite pedicle, or to impact loose fragments of bone anteriorly (Fig. 25.2)
Transpedicular Decompression
Description
Key Principles
Expectations
Indications
Contraindications
Special Considerations
Special Instructions, Position, and Anesthesia
Tips, Pearls, and Lessons Learned
Difficulties Encountered
Key Procedural Steps
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








